Chapter 8: Circadian Rhythms and Sleep
8.6: Brain structures involved in sleep
When scientists use an EEG to measure electrical activity, they look at the activity of neurons in the cortex, the outermost layer of brain cells. However, sleep and wake behaviors are driven by the action of cells that lie buried deep within the phylogenetically older areas of the brain. The signals that originate here communicate broadly throughout the rest of the brain, and these signals are the ones that cause us to sleep or wake. It is not just a single part of the brain that controls sleep behavior, but most likely a network of communication activity between different areas. Here, we will only address a few of the brain areas that are heavily involved with sleep.
Hypothalamus
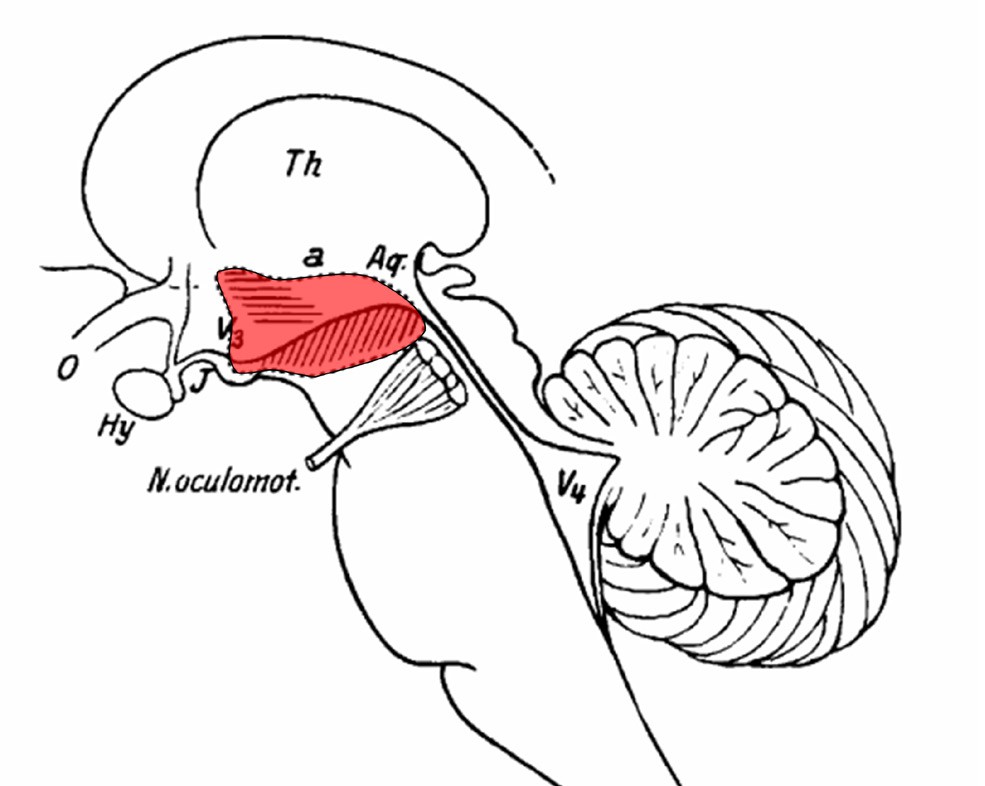
Early studies on the role of the hypothalamus in sleep began with Viennese neurologist, Constantin von Economo. He described a series of patients with a disease called encephalitis lethargica in 1917. In his observations, patients presented with one of two sets of symptoms. Some had progressive lethargy, starting with drowsiness, moving to extended sleeping periods, worsening to coma. On the complete opposite end of the spectrum, some patients had severe insomnia – a clinically
significant difficulty with falling asleep. When von Economo performed the autopsy on the patients, he found very specific injuries in the hypothalamus that correlated with symptoms. Among those with persistent sleepiness, the posterior hypothalamus was severely damaged. Von Economo concluded therefore that the posterior hypothalamus contained structures that are needed for maintenance of wakefulness in the healthy individual. In the patients with insomnia as their main symptom, their anterior hypothalamus was injured, leading von Economo to conclude that this area was important for promoting sleep.
Von Economo’s findings represented a shift in the way scientists thought of sleep. Most researchers believed that sleep was brought on simply by an overall decrease in brain activity. However, his discovery of hypothalamic localization of a “sleep center” demonstrated that for normal sleep to happen, certain areas in the anterior hypothalamus actually need to increase their activity.
The hypothalamus can be subdivided further into populations of neurons that have previously been addressed in some context. The suprachiasmatic nucleus (SCN), the neurons that receive light information via the retinohypothalamic tract and help regulate melatonin release, is part of the hypothalamus. Elsewhere in the hypothalamus is the tuberomammillary nucleus, the major site of neuronal production of the wakefulness signal histamine. The lateral hypothalamus has neurons that produce the pro-wakefulness signaling molecule orexin (sometimes also called hypocretin), and these neurons are lost in people with severe narcolepsy.
Clinical connection: Encephalitis lethargica
In the midst of World War I, a strange disease of unknown origin called encephalitis lethargica ravaged the globe. A worldwide pandemic, an estimated five million people were affected. About half of the patients died from early stage symptoms, and those who survived often failed to recover fully.
Encephalitis lethargica was also called “sleeping sickness” because of the symptoms that patients experienced: a lack of energy, extreme muscle weakness, and loss of all desires. Neurologist Oliver Sacks described these patients as being “insubstantial as ghosts, and as passive as zombies.”
Today, cases of encephalitis lethargica are extremely rare. The cause of the disease was never figured out, but one theory suggests that malfunctions in the immune system are related to the onset of the disease, since a major outbreak appeared in the wake of the Spanish flu pandemic of 1918.
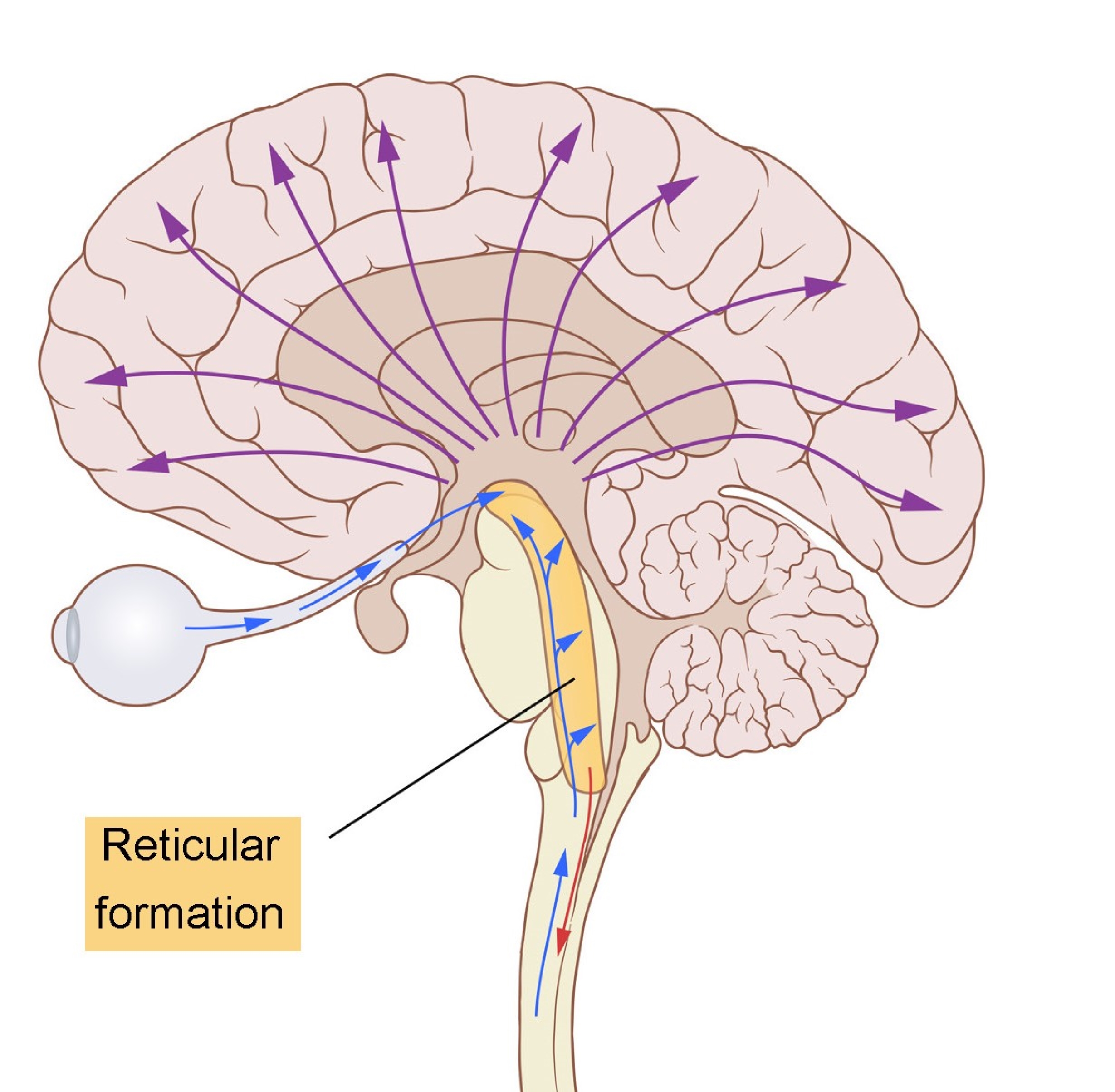
Reticular formation
The reticular formation is found in the brainstem. Like a large net of interconnected clumps of neurons, it is difficult to anatomically classify the structures of the reticular formation, since they do not have a clearly defined border or boundary. Activity of these neurons contribute to a variety of behavioral states, such as alertness and consciousness. The reticular formation is vulnerable to ischemia, lesions, or physical trauma. Often, severe injuries may result in a loss of consciousness or coma.
Information flow through the reticular formation passes in the upwards (towards the cortex) and downwards (towards the body) directions. The upward pathway, also called the ascending reticular activating system (ARAS), receives inputs from all the sensory systems before sending wide projections all across the cortex. (For your curiosity, the downward pathway is the reticulospinal tract that is involved with motor control of the skeletal muscles, and is not strongly involved with sleep behaviors.)