Chapter 14: Biopsychology of Psychological Disorders
Schizophrenia is a psychological disorder that is characterized by major disturbances in thought, perception, emotion, and behavior. About 1% of the population experiences schizophrenia in their lifetime, and the disorder is usually first diagnosed during early adulthood (early to mid-20s). Many people with schizophrenia report significant difficulties in some day-to-day activities, such as holding a job, paying bills, caring for oneself, and maintaining relationships with others. Although presentation of schizophrenia varies widely, symptoms of schizophrenia fall into three categories: 1) positive symptoms (symptoms that are “added”), which include hallucinations and delusions; 2) negative symptoms (symptoms that are “subtracted” or taken away), which include flat affect and social withdrawal; and 3) disorganized symptoms, which include disorganized speech and behavior (APA, 2022).
A hallucination is a perceptual experience that occurs in the absence of external stimulation. Auditory hallucinations (e.g., hearing voices) occur in roughly two-thirds of patients with schizophrenia and are by far the most common form of hallucination (Andreasen, 1987).
Delusions are beliefs that are contrary to reality and are firmly held even in the face of contradictory evidence. Paranoid delusions refer to the (false) belief that other people are plotting to harm them. For example, someone with schizophrenia may believe that their mother is plotting with the FBI to poison their coffee. People with schizophrenia also may hold grandiose delusions, which refer to beliefs that one holds special power, unique knowledge, or is extremely important (e.g., claiming to be Jesus Christ or be a great philosopher). Another type of delusion is somatic delusion, which is the belief that something highly abnormal is happening to one’s body (e.g., that one’s kidneys are being eaten by cockroaches).
Negative symptoms refer to a reduction or absence of normal behaviors related to motivation, interest, or expression (Correll & Schooler, 2020). Negative symptoms of schizophrenia include withdrawal from social relationships, reduced speaking, blunted emotion, and reduced experience of pleasure.
Disorganized thinking refers to disjointed and incoherent thought processes—usually detected by what a person says. The person might ramble, exhibit loose associations (jump from topic to topic), or talk in a way that is so disorganized and incomprehensible that it seems as though the person is randomly combining words.
Disorganized or abnormal motor behavior refers to unusual behaviors and movements: becoming unusually active, exhibiting silly child-like behaviors (giggling and self-absorbed smiling), engaging in repeated and purposeless movements, or displaying odd facial expressions and gestures. In some cases, the person will exhibit catatonic behaviors, which show decreased reactivity to the environment, such as posturing, in which the person maintains a rigid and bizarre posture for long periods of time, or catatonic stupor, a complete lack of movement and verbal behavior.[1]
Neural mechanisms underlying schizophrenia
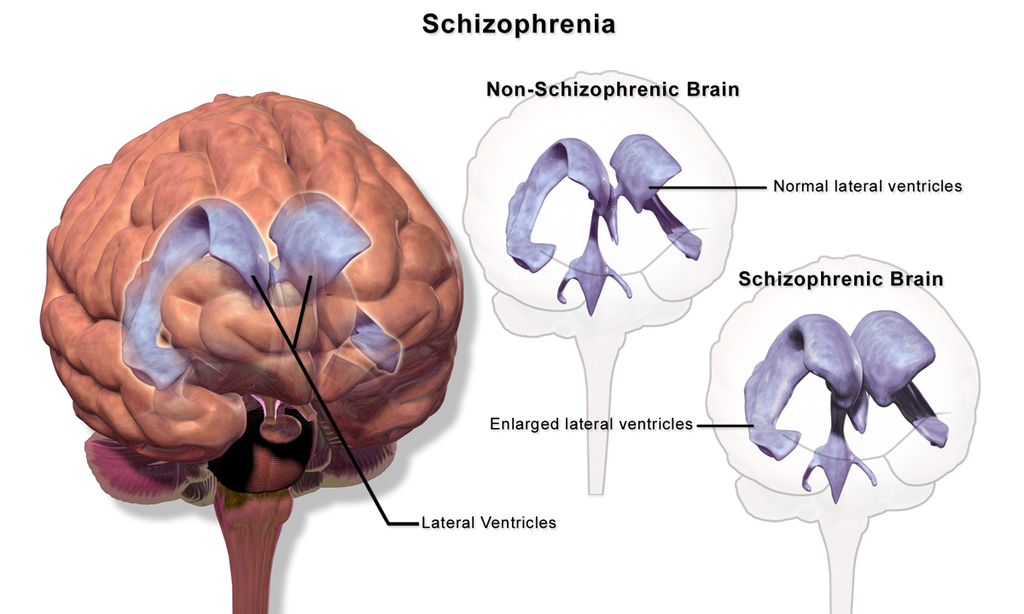
Scientists have identified several neural and biological signatures of schizophrenia. A highly consistent abnormality in brain structure in schizophrenia is enlarged ventricles (the cerebrospinal fluid-filled spaces in the brain). The ventricles in individuals with schizophrenia average around 30% larger than in controls, showing brain shrinkage in schizophrenia (Figure 14.6) (Horga et al., 2011). Individuals with schizophrenia tend to have smaller brain volumes of some subcortical structures including the hippocampus, amygdala, and thalamus (van Erp et al., 2016) and thinner cortex especially in the frontal and temporal lobe regions (van Erp et al., 2018). Functional neuroimaging studies have shown that patients with schizophrenia display hyperactivity in the hippocampus, a neural structure involved in learning and memory (Kraguljac et al., 2021). This hippocampal hyperactivity is thought to result in downstream dopamine circuit dysregulation, which may contribute to distorted interpretations of salience seen in individuals with schizophrenia. Dopamine dysregulation is one of the most prominent neural mechanisms underlying schizophrenia, and as a result, the most common schizophrenia medications target dopaminergic circuitry. In the rest of this section, we discuss the dopamine hypothesis and stress response in schizophrenia.
One of the earliest, and perhaps most influential, biological accounts of schizophrenia is the “dopamine hypothesis of schizophrenia.” The dopamine hypothesis suggests that excessive dopamine activity may be related to schizophrenia (Meltzer & Stahl, 1976). This account was originally inspired by seminal work showing that drugs that decrease dopamine activity may reduce symptoms related to schizophrenia, and drugs that enhance dopamine activity may increase symptoms (Carlsson & Lindqvist, 1963). The dopamine hypothesis has undergone several iterations.
The second iteration of the dopamine hypothesis of schizophrenia (Dopamine Hypothesis: Version II) proposed that schizophrenia does not simply stem from excess dopamine throughout the brain, but rather from region-specific dopamine activity. Researchers proposed distinctions between cortical and subcortical dopamine levels for negative and positive symptoms. Reduced dopaminergic engagement in the frontal cortex was linked to negative symptoms (e.g., social and emotional withdrawal) (Davis et al., 1991), whereas hyperactive dopaminergic engagement in the subcortical striatum was linked to positive symptoms (i.e., delusions, hallucinations) (Pycock et al., 1980). Ultimately, the Version II hypothesis proposed that reduced dopaminergic engagement in prefrontal areas led to hyperactive dopaminergic engagement in striatal areas, which contributed to the hallmark symptoms of schizophrenia.
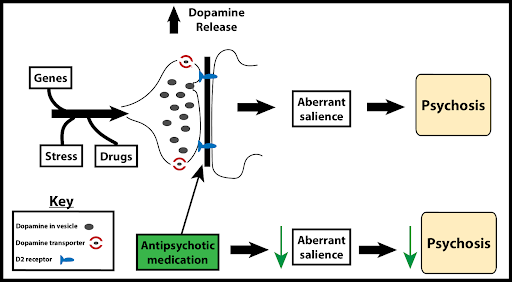
Version III of the dopamine hypothesis departs from previous hypotheses in several ways. First, it proposes that dopamine dysregulation may be less relevant to schizophrenia as a whole, and instead contributes specifically to acute psychosis (a brief period of delusion, hallucination, or disorganized thinking that dissociates the individual from reality) (Howes & Kapur, 2009). Psychotic symptoms, such as delusions and hallucinations, could emerge from excessive dopamine in the striatum (a subcortical structure involved in processing salience) that causes neutral items and events to be interpreted as overly important or salient (e.g., “aberrant salience”) (Figure 14.7) (Kapur et al., 2003).
Version III of the dopamine hypothesis also proposes that the main source of dopamine dysregulation may not be exclusively at the dopamine type D2 receptor level. In line with this perspective, recent work shows that newer treatments that target glutamatergic and dopaminergic mechanisms, other than D2 receptors, are also effective at reducing schizophrenia symptoms (Krystal, 2021). Version III also highlights other dimensions driving schizophrenia, such as the environmental, sociocultural, and genetic risk factors that impact dopamine dysregulation and their influence on cognitive dysfunction and symptom profiles.
Another influential account is the neural diathesis-stress model of schizophrenia, which proposes that schizophrenia may result from an interaction between preexisting vulnerabilities (“diathesis” means vulnerability or predisposition) and stress caused by life experiences. As discussed in Chapter 8, schizophrenia is highly heritable and has a strong genetic component (people with a close genetic relative with schizophrenia, like a parent, sibling, or twin, are more likely to develop schizophrenia); however, genetically predisposed individuals are far more likely to develop schizophrenia if they experience significant life stress—the stressful events can trigger or catalyze the development of the disorder.
Seminal work on neural diathesis-stress model of schizophrenia notes that stress worsens symptoms of schizophrenia and that the diathesis (or predisposition) is marked by a heightened stress response (Walker & Diforio, 1997). The model proposes that the hypothalamic-pituitary-adrenal gland (HPA) axis releases the hormone cortisol in response to stress and may mediate the effects of stress on schizophrenia symptoms. HPA-axis dysfunction may arise from hippocampal abnormalities in schizophrenia, exacerbate dopamine neurotransmission, and render a hypersensitivity to stress. Together, hippocampal, HPA axis, and dopamine dysfunction are thought to collectively promote a heightened stress response that marks a vulnerability to schizophrenia. To combat effects of stress, researchers highlight resilience or protective factors, including social support, self-esteem, coping skills, and antipsychotic medication (Pruessner et al., 2017).
While we focus here on the diathesis-stress model for schizophrenia, it is important to note that diathesis-stress models (i.e., the important interaction between predisposition and stressful life events) also apply to other psychological disorders such as depression and anxiety (Arnau-Soler et al., 2019).
- This section contains material adapted from: Spielman, R. M., Jenkins, W. J., & Lovett, M. D. (2020). 15.8 Schizophrenia. In Psychology 2e. OpenStax. Access for free at https://openstax.org/books/psychology-2e/pages/15-8-schizophrenia License: CC BY 4.0 DEED. ↵
Schizophrenia is a psychological disorder characterized by major disturbances in thought, perception, emotion, and behavior. Major symptoms include hallucinations, delusions, disorganized thinking, abnormal motor behavior, and negative symptoms.
Perceptual experience that emerges in the absence of external stimulation. Extends across different sensory sources (i.e., visual, auditory, tactile, etc.)
False beliefs that are contrary to external reality and are firmly held despite contrary evidence
Characterized by intense irrational thoughts and fears centered on perceived victimization or belief that one is being persecuted
Characterized by intense irrational thoughts and fears centered on perceived victimization or belief that one is being persecuted
Characterized by false beliefs that a person’s internal or external bodily functions are abnormal
Refer to an absence or reduction of normal behaviors related to motivation and interest, such as social withdrawal, diminished affective response, lack of interest.
Prominent feature of Schizophrenia; characterized by a pattern of incoherent and illogical thought processes
Prominent feature of Schizophrenia; characterized by extremely disjointed and atypical motor behavior that can cause problems in everyday life, ranging from childlike silliness to unpredictable agitation
Subtype of disorganized or abnormal motor behavior; involves significant reductions in voluntary movement and reduced reactivity to environmental stimulation
An enduring account that suggests a dysregulated dopamine system contributes to symptomatology of schizophrenia; has undergone many iterations
Neurotransmitter involved in learning, motivation, and reward. Implicated in schizophrenia
Stress, through its effects on cortisol, acts upon a pre-existing vulnerability to trigger or worsen schizophrenia symptoms.
