5 Birth and the Newborn
Learning Objectives
After reading Chapter 5, you should be better equipped to:
- Compare and contrast different methods of childbirth preparation.
- Describe the stages of vaginal delivery.
- Explain why induction or Caesarean section may be necessary.
- Differentiate the common procedures for assessing the condition of the newborn.
- Examine problems newborns experience before, during, and after birth.
- Explain the merits of breastfeeding.
- Discuss nutritional concerns of marasmus and kwashiorkor
Preparing for Childbirth
Prepared childbirth refers to being not only in good physical condition to help provide a healthy environment for the baby to develop, but also helping individuals to prepare to accept their new roles as parents. Additionally, parents can receive information and training that will assist them for delivery and life with the baby. The more future parents can learn about childbirth and the newborn, the better prepared they will be for the adjustment they must make to a new life. [1]
Choosing Where to Have the Baby and Who Will Deliver
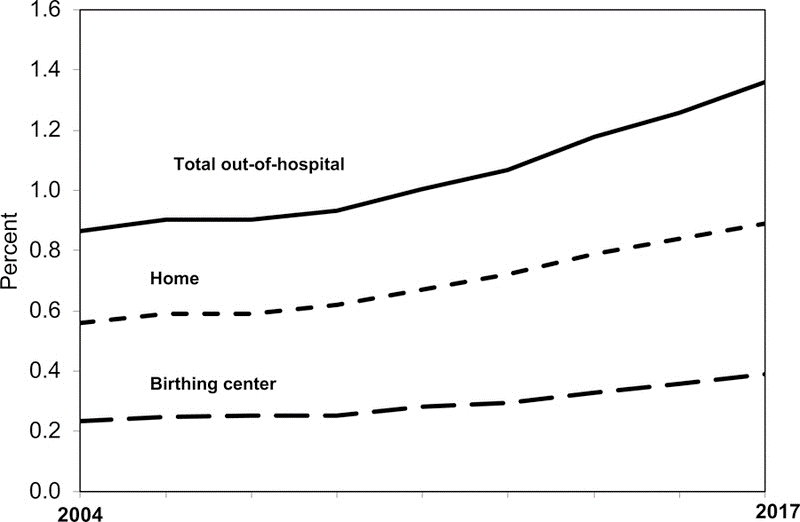
The vast majority of women in the United States give birth in a hospital (nearly 98.4%), but rates of home and birth center births are increasing, particularly in certain states and among certain populations. After a gradual decline from 1990–2004, the number of out-of-hospital births increased from 35,578 in 2004 to 62,228 in 2017. In 2017, 1 of every 62 births in the US was an out-of-hospital birth (1.64%). Home births increased by 77% from 2004–2017, while birth center births more than doubled. Out-of-hospital births were more common in the Pacific Northwest, and less common in the southeastern states such as Alabama, Louisiana, and Mississippi. Women with planned home and birth center births were less likely to have a number of population characteristics associated with poor pregnancy outcomes, including teen births, smoking during pregnancy, obesity, and preterm, low birthweight, and multiple births. More than two thirds of planned home births were self-paid, compared to 1/3 of birth center and just 3% of hospital births, with large variations by state.
Several states in the Northwestern part of the country, as well as one Eastern state had out-of-hospital birth rates above 3%, including Alaska (7.88%), Montana (4.08%), Idaho (3.77%) Washington (3.77%), Oregon (3.58%) and Pennsylvania (3.53%). In contrast, several other states had out-of-hospital birth rates from 0.4–0.6%: Alabama, Louisiana, Mississippi, Nebraska, New Jersey, and Rhode Island.
Home births were most common in Montana (2.74%), Vermont (2.56%), Wyoming (2.32%), Idaho (2.27%), Washington (2.14%), Wisconsin (2.10%), Oregon (2.10%), and Utah (2.04%), while home births were least common (below 0.5%) in Alabama, Louisiana, Mississippi, Nebraska, New Jersey, and Rhode Island.
Birth centers are available in most, but not all states. Twelve states (Alabama, Hawaii, Illinois, Iowa, Mississippi, Nevada, New Jersey, North Dakota, Rhode Island, South Dakota, Vermont and Wyoming) had fewer than 20 birth center births in 2017, suggesting that birth centers were not an available option for women living in those states. Among states with at least 20 birth center births in 2017, Alaska had the highest percentage of births occurring in a birth center (5.64%), followed by Washington (1.54%), Idaho (1.44%), Oregon (1.40%), Montana (1.34%), Delaware (1.29%), Pennsylvania (1.24%) and New Hampshire (1.00%).[2]
Women who are at low risk for birth complications can successfully deliver at home. More than half (67%) of home deliveries are assisted by certified nurse midwifes. Midwives are trained and licensed to assist in delivery and are far less expensive than the cost of a hospital delivery. However, because of the potential for a complication during the birth process, most medical professionals recommend that delivery take place in a hospital. Despite the concerns, in the United States women who have had previous children, who are over 25, and who are white are more likely to have out-of-hospital births (MacDorman, Menacker, & Declercq, 2010). In addition to home births, one-third of out-of-hospital births occur in freestanding clinics, birthing centers, in physician’s offices, or other locations.[3]
Percentage of Births Occurring Out-of-Hospital in the United States Between 2004 and 2017
While home births are still much less common than hospital births, recent data from the National Institute of Health (2020) notes that home births in the United States have increased 13% from 45,646 in 2020 to 51,642 in 2021. This increase followed a 19% rise in the number of home births from 2019 (38,506) to 2020. [4]
Percentage of Home Births by Race and Hispanic Origin of the Mother: United States, 2019-2020
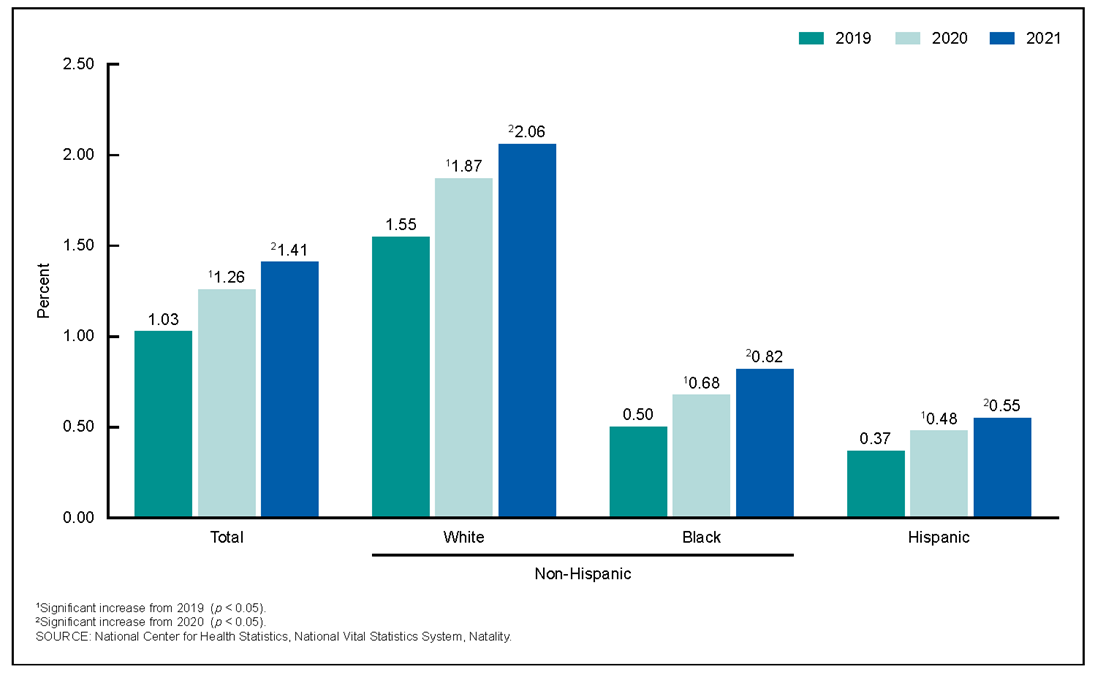
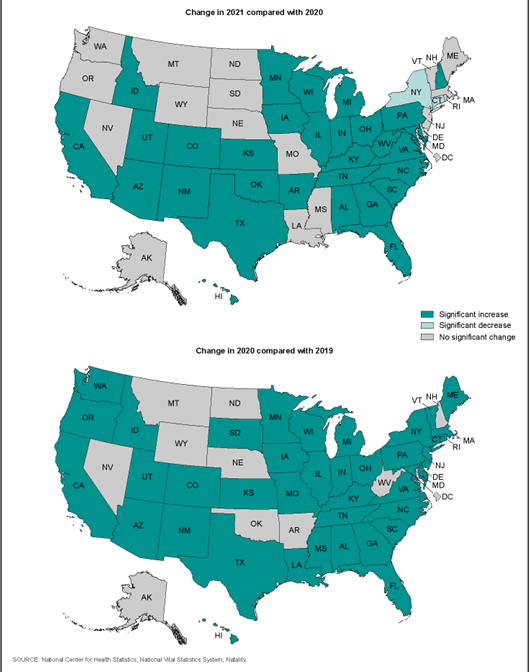
Home births increased in 30 states (with nonsignificant increases for 11 additional states) and declined in 2 states (with nonsignificant declines for 7 additional states and D.C.). The 12% increase in home births from 2020 to 2021 follows a 22% increase from 2019 to 2020, with increases by maternal race and Hispanic origin ranging from 21% to 36%. Home births increased for 40 states, with nonsignificant increases seen for 9 additional states and D.C. from 2019 to 2020.[5]
Approaches to Childbirth
There are many different approaches to childbirth that influence how expectant parents prepare. The two most common approaches to childbirth in the United States are the Lamaze method and the Bradley method.[6]
While both the Lamaze method and the Bradley method differ in their philosophy and focus each prepares the mother for natural childbirth. The Lamaze method emphasizes teaching the woman to be in control of the process of delivery, and to view childbirth as a natural process. While Lamaze classes do not discourage or support the use of medical intervention during childbirth, expecting moms are taught to reduce the pain associated with labor by using techniques such as, muscle relaxation, breathing through contractions, and having a focal point (usually a picture to look at) of concentration to distract from the pain of labor. In addition, the Lamaze technique suggests that a support person go through the six to eight week training classes with the mom and be prepared to serve as a coach during delivery process.
On the other hand, the Bradley method or husband-coached birth focuses on preparing the mother to deliver without the use of medical interventions. Like the Lamaze method, the Bradley method focuses on reducing pain and staying relaxed. Father’s play a much more active role in the coaching process than in the Lamaze method, and Dads are expected to practice breathing and massage techniques with their partner.[7]
Additional Approaches to Childbirth[8]
| Method | Description |
| The Leboyer Method | This method involves giving birth in a quiet, dimly lit room and allowing the newborn to lie on the mother’s stomach with the umbilical cord intact for several minutes while being given a warm bath. |
| Dick-Read Method | This method comes from the suggestion that the fear of childbirth increases tension and makes the process of childbearing more painful. It emphasizes the use of relaxation and proper breathing with contractions as well as family support and education. This method influenced the Lamaze method of childbirth. |
| Alexander Technique | This is a technique that can be used during childbirth that involves training to stop habitual reactions to pain, such as tensing muscles and increase conscious awareness and control over posture and movement. This involves being able to move freely and stay upright during labor and using body positioning that is beneficial to the labor process.[9] |
| Waterbirth | Involves immersion in warm water. Proponents believe this method is safe and provides many benefits for both mother and infant, including pain relief and a less traumatic birth experience for the baby. However, critics argue that the procedure introduces unnecessary risks to the infant such as infection and water inhalation.[10] |
| Lotus Birth | Or umbilical cord nonseverance – UCNS, is the practice of leaving the umbilical cord uncut after childbirth so that the baby is left attached to the placenta until the cord naturally separates at the umbilicus. This usually occurs within 3–10 days after birth. The practice is performed mainly for spiritual purposes of the parents, including for the perceived spiritual connection between placenta and newborn.[11] |
| Silent Birth | Sometimes known as quiet birth, is a birthing procedure advised by L. Ron Hubbard and advocated by Scientologists in which “everyone attending the birth should refrain from spoken words as much as possible.”[12] |
Expectant Parents Attending a Childbirth Preparation Class[13]

Test Yourself:
Childbirth
Onset of Labor
Childbirth typically occurs within a week of a woman’s due date, unless the woman is pregnant with more than one fetus, which usually causes her to go into labor early. As a pregnancy progresses into its final weeks, several physiological changes occur in response to hormones that trigger labor.
A common sign that labor is beginning is the so-called bloody show. During pregnancy, a plug of mucus accumulates in the cervical canal, blocking the entrance to the uterus. Approximately 1–2 days prior to the onset of true labor, this plug loosens and is expelled, along with a small amount of blood.
As labor nears, the mothers’ pituitary gland produces oxytocin. This begins to stimulate stronger, more painful uterine contractions, which—in a positive feedback loop—stimulate the secretion of prostaglandins from fetal membranes. Like oxytocin, prostaglandins also enhance uterine contractile strength. The fetal pituitary gland also secretes oxytocin, which increases prostaglandins even further. In addition, the stretching of the cervix by a full-term fetus in the head-down position is regarded as a stimulant to uterine contractions. Combined, these stimulate true labor.[14]
The First Stage of labor begins with uterine contractions that initially, may last about 30 seconds and be spaced 15 to 20 minutes apart. These increase in duration and frequency to more than a minute in length and about 3 to 4 minutes apart. Typically, doctors advise that they be called when contractions are coming about every 5 minutes. Some women experience false labor or Braxton-Hicks contractions, especially with the first child. These may come and go. They tend to diminish when the mother begins walking around. Real labor pains tend to increase with walking. Labor may also be signaled by a bloody discharge being expelled from the cervix. In one out of 8 pregnancies, the amniotic sac or water in which the fetus is suspended may break before labor begins. In such cases, the physician may induce labor with the use of medication if it does not begin on its own in order to reduce the risk of infection. Normally this sac does not rupture until the later stages of labor.
The first stage of labor is typically the longest. During this stage the cervix or opening to the uterus dilates to 10 centimeters or just under 4 inches (See figure below). This may take around 12-16 hours for first children or about 6-9 hours for women who have previously given birth. Labor may also begin with a discharge of blood or amniotic fluid.[15]
Stage One of the Birthing Process
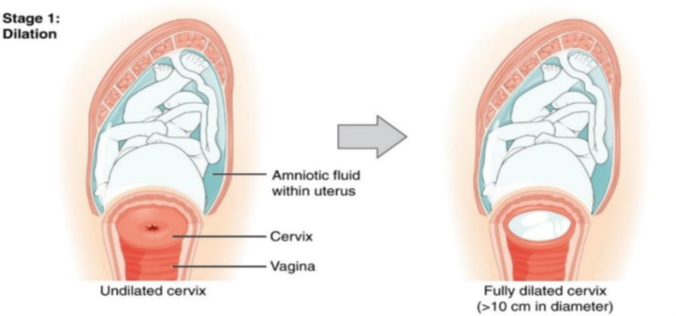
Early cervical dilation is shown on the left and the cervix when fully dilated on the right. [16]
The Second Stage
The passage of the baby through the birth canal is the second stage of labor. This stage takes about 10-40 minutes. Contractions usually come about every 2-3 minutes. The mother pushes and relaxes as directed by the medical staff. Normally the head is delivered first. The baby is then rotated so that one shoulder can come through and then the other shoulder. The rest of the baby quickly passes through. At this stage, an episiotomy, or incision made in the tissue between the vaginal opening and anus, may be performed to avoid tearing the tissue of the back of the vaginal opening (Mayo Clinic, 2016). The baby’s mouth and nose are suctioned out. The umbilical cord is clamped and cut.[17]
Stage Two of the Birthing Process
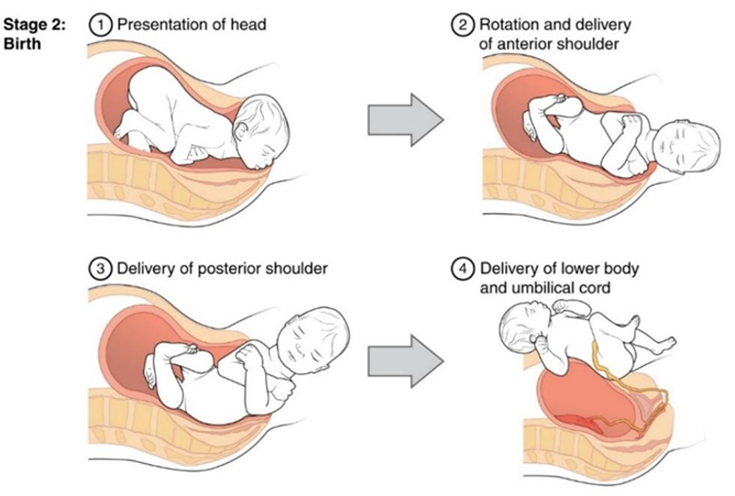
Full dilation and expulsion of the newborn[18]
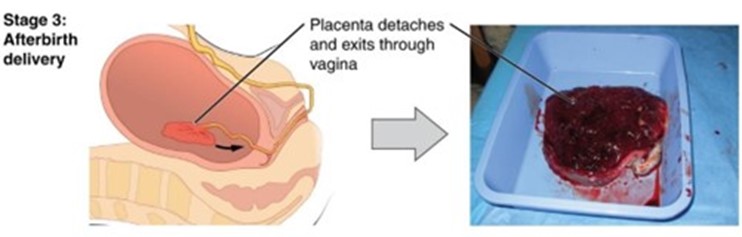
The Third Stage
The third of labor is relatively painless. During this stage, the placenta or afterbirth is delivered. This is typically within 20 minutes after delivery. If an episiotomy was performed it is stitched up during this stage.[19]
Stage Three of the Birthing Process
Pain Medications
More than 50% of women giving birth at hospitals use an epidural anesthesia during delivery (American Pregnancy Association, 2015). An epidural block is a regional analgesic that can be used during labor and alleviates most pain in the lower body without slowing labor. The epidural block can be used throughout labor and has little to no effect on the baby. Medication is injected into a small space outside the spinal cord in the lower back. It takes 10 to 20 minutes for the medication to take effect. An epidural block with stronger medications, such as anesthetics, can be used shortly before a Cesarean Section or if a vaginal birth requires the use of forceps or vacuum extraction.[20]
Women giving birth can also receive other pain medications (although medications given through injection can have negative side effects on the baby). If a mother is close to giving birth, a pudendal block can be administered during the second stage of labor just before delivery of the baby. A pudendal block will relieve the pain around the vagina and rectum as the baby comes down the birth canal, and is also helpful just before an episiotomy. In emergency situations (such as the need for a C-section), women may be given general anesthesia. They can also choose not to utilize any pain medications. That is often referred to as natural childbirth. Women can also use alternate positions during labor and birth (including standing, squatting, being on hands and knees, and using a birthing stool), including delivering in tubs of warm water to help relieve the pain of childbirth.
Giving Birth in a Water Tank (Hydrotherapy)[21]

Test Yourself:
Medical Interventions in Childbirth
Sometimes women cannot go into labor on their own and/or deliver vaginally. Let’s look at induction of labor and Cesarean Sections.
Sometimes a baby’s arrival may need to be induced before labor begins naturally. Induction of labor may be recommended for a variety of reasons when there is concern for the health of the mother or baby. For example:
- The mother is approaching two weeks beyond her due date and labor has not started naturally
- The mother’s water has broken, but contractions have not begun
- There is an infection in the mother’s uterus
- The baby has stopped growing at the expected pace
- There is not enough amniotic fluid surrounding the baby
- The placenta peels away, either partially or completely, from the inner wall of the uterus before delivery
- The mother has a medical condition that might put her or her baby at risk, such as high blood pressure or diabetes (Mayo Clinic, 2014).
Inducing Labor: There are both pharmacological and procedural methods in which labor can be induced. The most common is to intravenously administer a synthetic version of oxytocin called Pitocin. Once administered to the mom, the amount of Pitocin is adjusted based on whether or not contractions begin or become too fast or strong. Both the mom’s contractions and baby’s heart rate are continuously monitored while Pitocin is being administered.
Pitocin will not be administered, however unless the condition of the cervix is found to be “favorable.” The obstetrician will determine whether or not the cervix is ready by calculating a Bishop Score. There are five measures that are considered by one’s obstetrician when calculating the Bishop Score, which include (1) cervical dilation in centimeters, (2) cervical effacement or a measure of how thin the cervix has become, (3) cervical consistency (firm or soft), (4) cervical position, and (5) station, or the position of the fetal head in relation to the pelvic bones.[22]
Bishop Scoring
| Score | Dilation in cm | Effacement % | Cervical Consistency | Cervical Position | Station |
| 0 | Closed | 0-30% | Firm | Posterior | -3 |
| 1 | 1-2 cm | 40-50% | Medium | Mid Position | -2 |
| 2 | 3-4 cm | 60-70% | Soft | Anterior | -1 |
| 3 | >5 | >80% | —– | —– | 1, 2 |
(1) Dilation is a measure of how open the cervix is. (2) Effacement refers to how thin the cervix is. The cervix is approximately three centimeters long and during labor will efface until it paper thin. (3) The consistency of the cervix is tough and resistant to stretching but will become less rigid with each successive pregnancy. (4) The position of the cervix tends to become more anterior (nearer the opening of the vagina) as labor becomes closer. (5) Fetal station describes the position of the fetus’s head in relation to the distance from the ischial spines, which are approximately 3-4 centimeters inside the vagina and are not usually felt. Health professionals visualize where these spines are and use them as a reference point. Negative numbers indicate that the head is further inside than the ischial spines and positive numbers show that the head is below the level of the ischial spines. [23]
A Bishop Score of 8 or more indicates that labor will more than likely begin spontaneously, and if induction is needed, it most likely will be successful. A score between 6 and 7 cannot be used to make predictions regarding the success of labor or induction. A score of 5 or less is an indication that inducing labor may fail, and in this case the cervix may need to be “ripened.” [24]
Cervical ripening (CR), often an initial component of labor induction, is the process of softening and effacing the cervix as well as stimulating early cervical dilation. Based on data from trials of labor induction, approximately 83 to 85 percent of women with an indication for induction require cervical ripening. Common CR methods include pharmacologic options, such as prostaglandins (misoprostol and Prostaglandin E2), and mechanical options, such as inflating a balloon catheter in the cervix.
While prostaglandins (vaginal or oral) and mechanical methods (e.g. balloon catheters) are the most commonly used methods of CR in the inpatient setting, there is variation in the dose, regimen, or protocols applied. Some women’s cervixes will rapidly respond to a CR intervention, while others require extended time with more than one intervention being tried if the first one fails.[25]
Amniotomy: Amniotomy, also known as artificial rupture of membranes (AROM) and by the lay description “breaking the water,” is the intentional rupture of the amniotic sac by an obstetrical provider. This procedure is common during labor management and has been performed by obstetrical providers for at least a few hundred years. The reasons for the intentional rupture of the amniotic sac during labor are multifold and include, but are not limited to, influencing the speed of labor, allowing for more direct monitoring of fetal status, and qualitative assessment of the amniotic fluid.
Amniotomy is easily performed with the use of specially designed hooks intended to grab and tear the amniotic membrane. The two most used devices are (1) an approximately 10-inch rod with a hook on the end of the rod or (2) a finger cot with a hook on the end of the cot. With either device, the practitioner first assesses cervical dilation through the performance of a sterile digital exam. At the same time, assessment of the fetal presenting part is made, ensuring that the presenting part is, in fact, the fetal head and assessing that the fetal head is well engaged in the pelvis. After confirmation of both fetal presentation and engagement, the practitioner can proceed with artificial rupture of membranes.[26]
A Cesarean Section (C-section) is surgery to deliver the baby by being removed through the mother’s abdomen. In the United States, about one in three women have their babies delivered this way (Martin et al., 2015). Most C-sections are done when problems occur during delivery unexpectedly. These can include:
- Health problems in the mother
- Signs of distress in the baby
- Not enough room for the baby to go through the vagina
- The position of the baby, such as a breech presentation where the head is not in the downward position.
Giving Birth via C-Section
C-sections are also more common among women carrying more than one baby. Although the surgery is relatively safe for mother and baby, it is considered major surgery and carries health risks. Additionally, it also takes longer to recover from a C-section than from vaginal birth. After healing, the incision may leave a weak spot in the wall of the uterus. This could cause problems with an attempted vaginal birth later. In the past, doctors were hesitant to allow a vaginal birth after a C-section. However, now more than half of women who have a C-section go on to have a vaginal birth later.[29] This is referred to as a Vaginal Birth After Cesarean (VBAC).[30]
Test Yourself:
The Newborn
Assessing the Newborn
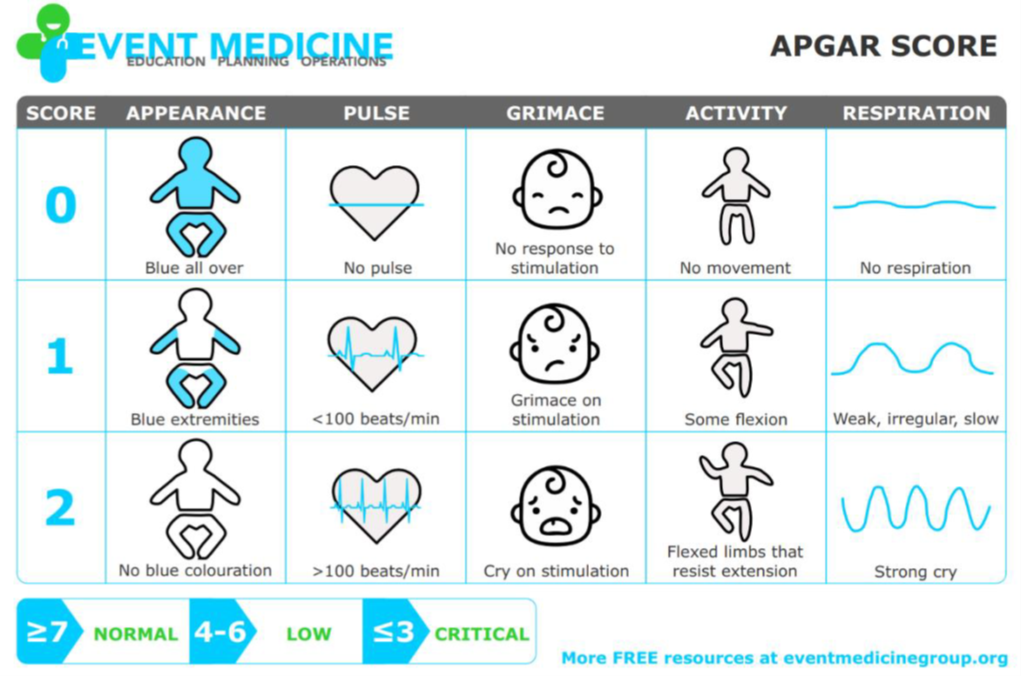
In the minutes following birth, a newborn must undergo dramatic systemic changes to be able to survive outside the womb. An obstetrician, midwife, or nurse can estimate how well a newborn is doing by obtaining an APGAR score. The Apgar score was introduced in 1952 by anesthesiologist Dr. Virginia Apgar as a method to assess the effects on the newborn of anesthesia given to the laboring mother. Healthcare providers now use it to assess the general wellbeing of the newborn, whether or not analgesics or anesthetics were used.
Five criteria are assessed:
- Skin color
- Heart rate
- Reflex,
- Muscle tone
- Respiration
Each criterion is assigned a score of 0, 1, or 2. Scores are taken at 1 minute after birth and again at 5 minutes after birth. Each time that scores are taken, the five scores are added together. High scores (out of a possible 10) indicate the baby has made the transition from the womb well, whereas lower scores indicate that the baby may be in distress. The technique for determining an APGAR score is quick and easy, painless for the newborn, and does not require any instruments except for a stethoscope.
Of the five APGAR criteria, heart rate and respiration are the most critical. Poor scores for either of these measurements may indicate the need for immediate medical attention to resuscitate or stabilize the newborn. In general, any score lower than 7 at the 5-minute mark indicates that medical assistance may be needed. A total score below 5 indicates an emergency situation. Normally, a newborn will get an intermediate score of 1 for some of the APGAR criteria and will progress to a 2 by the 5-minute assessment. Scores of 8 or above are normal.[31]
The APGAR Assessment[32]
Another way to assess the condition of the newborn is by administering the Neonatal Behavioral Assessment Scale (NBAS) developed by Brazelton in the 70’s. This Scale contains 28 behavioral and 18 reflex items, that assess the baby’s capabilities across different developmental areas (autonomic, motor, state, and social-interactive systems) and describes how infants integrate these areas as they adapt to their new environment. At the time it was developed in the 70’s the approach was considered innovative for recognizing that a baby is a highly developed organism, even when just newly born. Today, this tool has been used around the world to further assess the newborn, especially those with low Apgar scores, and to make comparisons of infants in different cultures (Brazelton & Nugent, 1995). [33]
In addition to the Apgar and the Neonatal Behavioral Assessment, newborns are also routinely screened for different conditions. Within the first 24 to 48 hours after birth, babies born in hospitals undergo a simple heel stick test, where a few drops of blood are collected on a special paper card. Providers test those dried blood spots for a variety of different congenital disorders, or conditions that are present when the baby is born. In California, newborns are now screened for 80 different genetic and congenital disorders.
The Heel Stick Test

A medical professional performing the heel stick test.[34]
Newborns are also screened for hearing disorders and certain serious heart problems.[35]
Appearance at Birth
During labor and birth, the infant’s skull changes shape to fit through the birth canal, sometimes causing the child to be born with a misshapen or elongated head. It will usually return to normal on its own within a few days or weeks.
Some newborns have a fine, velvety body hair called lanugo. It may be particularly noticeable on the back, shoulders, forehead, ears and face of premature infants. Lanugo disappears within a few weeks. Likewise, not all infants are born with lush heads of hair. Some may be nearly bald while others may have very fine, almost invisible hair. Some babies are even born with a full head of hair. Amongst fair-skinned parents, this fine hair may be blond, even if the parents are not. The picture on the left shows lanugo on the shoulders of newborn twins.
Images of Lanugo and Vernix
 |
 |
| Lanugo on the shoulder and back of twin girls.[36] | A newborn baby covered in vernix.[37] |
Immediately after birth, a newborn’s skin is often grayish to dusky blue in color. As soon as the newborn begins to breathe, usually within a minute or two, the skin’s color returns to its normal tone. Newborns are wet, covered in streaks of blood, and coated with a white substance known as vernix, which is thought to act as an antibacterial barrier, seen in the picture on the right.
The scalp may also be temporarily bruised or swollen, especially in hairless newborns, and the area around the eyes may be puffy.[38]
The newborn may also have Mongolian spots (blue- or blue-black) birthmark on the lower back), various other birthmarks, or peeling skin, particularly on the wrists, hands, ankles, and feet. [39]
A newborn’s genitals are enlarged and reddened, with male infants having an unusually large scrotum. The breasts may also be enlarged, even in male infants. This is caused by naturally occurring maternal hormones and is a temporary condition.
The umbilical cord of a newborn is bluish-white in color. After birth, the umbilical cord is normally cut, leaving a 1–2-inch stub. The umbilical stub will dry out, shrivel, darken, and spontaneously fall off within about 3 weeks. Occasionally, hospitals may apply triple dye to the umbilical stub to prevent infection, which may temporarily color the stub and surrounding skin purple.
Cutting the Umbilical Cord

The clamping and cutting of a newborn’s umbilical cord. [40]
Newborns lose many of the above physical characteristics quickly. Thus older babies look very different. While older babies are considered “cute,” newborns can be “unattractive” by the same criteria and first time parents may need to be educated in this regard.[41]
Problems of the Newborn
Anoxia is a temporary lack of oxygen to the brain. Difficulty during delivery may lead to anoxia which can result in brain damage or in severe cases, death. Babies who suffer both low birth weight and anoxia are more likely to suffer learning disabilities later in life as well.
A child is considered low birth weight if he or she weighs less than 5 pounds 8 ounces (2500 grams) at birth. About 8.2 percent of babies born in the United States are of low birth weight (Center for Disease Control, 2015a). Sixty-seven percent of these babies are also preterm. A low birth weight baby has difficulty maintaining adequate body temperature because it lacks the fat that would otherwise provide insulation. Such a baby is also at more risk for infection. Very low birth weight babies (3 pounds, 4 ounces or less) have an increased risk of developing cerebral palsy. Many causes of low birth weight are preventable with proper prenatal care.
A newborn might also have a low birth weight if it is born at less than 37 weeks gestation, which qualifies the infant as a preterm baby (CDC, 2015c). Early birth can be triggered by anything that disrupts the mother’s system. For instance, vaginal infections can lead to premature birth because such infection causes the mother to release anti-inflammatory chemicals which, in turn, can trigger contractions. Smoking and the use of other teratogens can lead to preterm birth. A significant consequence of preterm birth includes respiratory distress syndrome, which is characterized by weak and irregular breathing (see the image below). Premature babies often cannot yet regulate their own temperature or feed by nursing or bottle. They may struggle to regulate their heart rate effectively and may experience jaundice. They often require care in the Neonatal Intensive Care Unit (NICU) until they are as healthy as a full-term baby.[42]
A Newborn in the NICU

A premature baby on a “Continuous Positive Airway Pressure” (CPAP) in the Neonatal Intensive Care Unit (NICU).[43]
Infants that have birth weights that are below expectation based on their gestational age are referred to as small-for-date. These infants may be full term or preterm (see image below), but still weigh less than 90% of all babies of the same gestational age. This is a very serious situation for newborns as their growth was adversely affected. Regev et al. (2003) found that small-for-date infants died at rates more than four times higher than other infants.
A Premature Infant Who is Also Very Low Birth Weight

The baby above was born at 32 weeks and only weighed 2 pounds and 15 ounces.[44]
When babies are not born by 42 weeks gestation, or two weeks after their due date, they are considered overdue or postmature. There are some concerns about how long the placenta can function and most doctors will consider induction for overdue babies.
When a fetus (unborn baby) dies while still inside the mother (after 20-24 weeks gestation) or dies during delivery (childbirth), it is said that the delivered baby is stillborn. The causes of many stillbirths are unknown, even when special tests are done to learn the cause. Possible causes include nicotine, alcohol, or drugs taken by the mother during pregnancy, physical trauma, radiation poisoning, Rh disease, and umbilical cord problems. The number of stillbirths in the United States is about 1 in 115 births, which is about 26,000 a year, or one every 20 minutes.[45]
Test Yourself
Breast Milk and Feeding
Breast milk is considered the ideal diet for newborns. It has the right amount of calories, fat, and protein to support overall physical and neurological development, provides a source of iron more easily absorbed in the body than the iron found in dietary supplements, provides a resistance against many diseases, is more easily digested by infants than is formula, and it helps babies make a transition to solid foods more easily than if bottle fed. For all these reasons, it is recommended that mothers breast feed their infants until at least 6 months of age and that breast milk be used in the diet throughout the first year (U.S. Department of Health and Human Services, 2004a in Berk, 2007). However, most mothers who breastfeed in the United States stop breast feeding at about 6-8 weeks, often to return to work outside the home. Mothers can certainly continue to provide breast milk to their babies by expressing and then freezing the milk to be bottle fed at a later time or by being available to their infants at feeding time. However, some mothers find that after the initial encouragement they receive in the hospital to breast feed, the outside world is less supportive of such efforts. Some workplaces support breastfeeding mothers by providing flexible schedules and welcoming infants, but many do not, and the public support of breastfeeding is sometimes lacking. Women in Canada are more likely to breastfeed than are those in the United States and the Canadian health recommendation is for breastfeeding to continue until 2 years of age. Facilities in public places in Canada such as malls, ferries, and workplaces provide more support and comfort for the breastfeeding mother and child than found in the United States.
One early argument given to promote the practice of breastfeeding was that it promoted bonding and healthy emotional development for infants. However, this does not seem to be the case. Breastfed and bottle-fed infants adjust equally well emotionally (Ferguson and Woodward, 1999). This is good news for mothers who may be unable to breastfeed for a variety of reasons and for fathers who might feel left out as a result.
In addition to the nutritional benefits of breastfeeding, breast milk is free! Anyone who has priced formula recently can appreciate this added incentive to breastfeeding. Prices for a month’s worth of formula can easily range from $130-200. Breastfeeding also stimulates contractions in the uterus to help it regain its normal size. And women who breastfeed are more likely to space their pregnancies further apart.
Counter arguments of breastfeeding:
Although there is research that promotes breastfeeding there are also those who challenge the belief that breast milk is free. For breastmilk to be completely beneficial for infants the mother’s life choices will ultimately affect the quality of the nutrition an infant will receive. Let’s consider the nutritional intake of the mother. Breastfeeding will both limit some food and drink choices as well as necessitate an increased intake of healthier options. A simple trip down the supermarket aisles will show you that nutritious and healthier options can be more expensive than some of the cheaper more processed options. A large variety of vegetable and fruits must be consumed, accompanied by the right proportions and portions of the whole grains, dairy products, and fat food groups. Additionally, it is also encouraged for breastfeeding mothers take vitamins regularly. That raises the question of how free breastfeeding truly is.
A historic look at breastfeeding:
The use of wet nurses, or lactating women hired to nurse others’ infants, during the middle ages eventually declined and mothers increasingly breastfed their own infants in the late 1800s. In the early part of the 20th century, breastfeeding began to go through another decline and by the 1950s, it was practiced less frequently by middle class, more affluent mothers as formula began to be viewed as superior to breast milk. In the late 1960s and 1970s, greater emphasis began to be placed on natural childbirth and breastfeeding and the benefits of breastfeeding were more widely publicized. Gradually rates of breastfeeding began to climb, particularly among middle-class educated mothers who received the strongest messages to breastfeed. Today, women receive consultation from lactation specialists before being discharged from the hospital to ensure that they are informed of the benefits of breastfeeding and given support and encouragement to get their infants to get used to taking the breast. This does not always happen immediately and first-time mothers, especially, can become upset or discouraged. In this case, lactation specialists and nursing staff can encourage the mother to keep trying until baby and mother are comfortable with the feeding.
Global Considerations and Malnutrition
In the 1960s, formula companies led campaigns in developing countries to encourage mothers to feed their babies on infant formula. Many mothers felt that formula would be superior to breast milk and began using formula. The use of formula can certainly be healthy under conditions in which there is adequate, clean water with which to mix the formula and adequate means to sanitize bottles and nipples. However, in many of these countries such conditions were not available, and babies often were given diluted, contaminated formula which made them become sick with diarrhea and become dehydrated. Rates of breast feeding declined in Peru from 90 percent to 10 percent in just 8 years’ time (Berger, 2001). These conditions continue today and now many hospitals prohibit the distribution of formula samples to new mothers in efforts to get them to rely on breast feeding. Many of these mothers do not understand the benefits of breast feeding and need to be encouraged and supported to promote this practice. Breast feeding could save the lives of millions of infants each year, according to the World Health Organization, yet fewer than 40 percent of infants are breastfed exclusively for the first 6 months of life.
Most women can breastfeed unless they are receiving chemotherapy or radiation therapy, have HIV, are dependent on illicit drugs, or have active, untreated tuberculosis.
Children in developing countries and countries experiencing the harsh conditions of war are at risk for two major types of malnutrition. Infantile marasmus refers to starvation due to a lack of calories and protein. Children who do not receive adequate nutrition lose fat and muscle until their bodies can no longer function. Babies who are breast fed are much less at risk of malnutrition than those who are bottle fed. After weaning, children who have diets deficient in protein may experience kwashiorkor or the “disease of the displaced child” often occurring after another child has been born and taken over breastfeeding. This results in a loss of appetite and swelling of the abdomen as the body begins to break down the vital organs as a source of protein.
The Breast Milk Industry: The benefits of breast milk are well-known and publicized. The collection and distribution of breast milk has become a million-dollar industry supplying hospitals and others in need of the ideal diet. For more information, go to www.prolacta.com to see a current development in the story of breast milk.
Milk Anemia in the United States: About 9 million children in the United States are malnourished (Children’s Welfare, 1998). More still suffer from milk anemia, a condition in which milk consumption leads to a lack of iron in the diet. This can be due to the practice of giving toddlers milk as a pacifier-when resting, when riding, when waking, and so on. Appetite declines somewhat during toddlerhood and a small amount of milk (especially with added chocolate syrup) can easily satisfy a child’s appetite for many hours. The calcium in milk interferes with the absorption of iron in the diet as well. Many preschools and daycare centers give toddlers a drink after they have finished their meal in order to prevent spoiling their appetites.[46]
Test Yourself:
Infant Sleep
A newborn typically sleeps approximately 16.5 hours per 24-hour period. This is usually polyphasic sleep in that the infant is accumulating the 16.5 hours over several sleep periods throughout the day (Salkind, 2005). The infant is averaging 15 hours per 24-hour period by one month, and 14 hours by 6 months. By the time children turn two, they are averaging closer to 10 hours per 24 hours. Additionally, the average newborn will spend close to 50% of the sleep time in the rapid eye movement (REM) phase, which decreases to 25% to 30% in childhood.
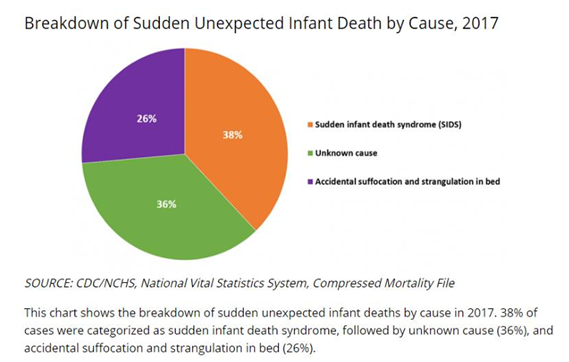
Sudden Unexpected Infant Deaths (SUID): Each year in the United States, there are about 3,500 Sudden Unexpected Infant Deaths (SUID). These deaths occur among infants less than one-year-old and have no immediately obvious cause (CDC, 2019). The three commonly reported types of SUID are:
- Sudden Infant Death Syndrome (SIDS): SIDS is identified when the death of a healthy infant occurs suddenly and unexpectedly, and medical and forensic investigation findings (including an autopsy) are inconclusive. SIDS is the leading cause of death in infants 1 to 12 months old, and approximately 1,400 infants died of SIDS in 2017 (CDC, 2019). Because SIDS is diagnosed when no other cause of death can be determined, possible causes of SIDS are regularly researched. One leading hypothesis suggests that infants who die from SIDS have abnormalities in the area of the brainstem responsible for regulating breathing (Weekes-Shackelford & Shackelford, 2005).
- Unknown Cause: The sudden death of an infant less than one year of age that cannot be explained because a thorough investigation was not conducted, and cause of death could not be determined. In 2017, 1300 infants died from unknown causes (CDC, 2019).
- Accidental Suffocation and Strangulation in Bed: Reasons for accidental suffocation include: Suffocation by soft bedding, another person rolling on top of or against the infant while sleeping, an infant being wedged between two objects such as a mattress and wall, and strangulation such as when an infant’s head and neck become caught between crib railings. In 2017, 900 infants died from accidental suffocation and strangulation. The 2017 percentages of infants who died based on each of the three types are listed in the pie chart below.[47]
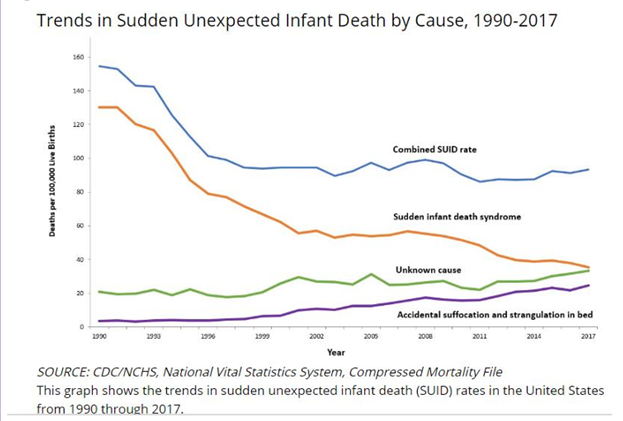
As can be seen in the following line graph, the combined SUID death rate declined considerably following the release of the American Academy of Pediatrics safe sleep recommendations in 1992, which advocated that infants be placed for sleep on their backs (nonprone position). These recommendations were followed by a major Back to Sleep Campaign in 1994. However, accidental suffocation and strangulation in bed mortality rates remained unchanged until the late 1990s. In 1998 death rates from accidental suffocation and strangulation in bed actually started to increase, and they reached the highest rate at 24.6 deaths per 100,000 live births in 2017 (CDC, 2019).[48]
Should infants be sharing the bed with parents? Colvin, Collie-Akers, Schunn and Moon (2014) analyzed a total of 8207 deaths from 24 states during 2004–2012 that were contained in the National Center for the Review and Prevention of Child Deaths Case Reporting System, a database of death reports from state child death review teams. The results indicated that younger victims (0-3 months) were more likely to die by bed-sharing and sleeping in an adult bed/on a person. A higher percentage of older victims (4 months to 364 days) rolled into objects in the sleep environment and changed position from side/back to prone. Carpenter et al. (2013) compared infants who died of SIDS with a matched control and found that infants younger than three months old who slept in bed with a parent were five times more likely to die of SIDS compared to babies who slept separately from the parents but were still in the same room. They concluded that bed sharing, even when the parents do not smoke or take alcohol or drugs, increases the risk of SIDS. However, when combined with parental smoking and maternal alcohol consumption and/or drug use, risks associated with bed sharing greatly increased.
The two studies discussed above were based on American statistics. What about the rest of the world? Co-sleeping occurs in many cultures, primarily because of a more collectivist perspective that encourages a close parent-child bond and interdependent relationship (Morelli, Rogoff, Oppenheim, & Goldsmith, 1992). In countries where co-sleeping is common, however, 77% of parents and infants typically sleep on floor mats and other hard surfaces which minimize the suffocation that can occur with bedding (Nelson, Schiefenhoevel, & Haimerl, 2000).[49]
Test Yourself:
Postpartum Maternal Concerns
After pregnancy many women experience emotional changes. The baby blues are often mentioned as a common occurrence in new mothers. The baby blues are feelings of sadness that occur 3 to 5 days after having a baby, and typically disappear usually within 10 days of the birth. New mothers may have trouble sleeping, be moody, and feel let-down from the birthing experience. However, postpartum depression is not the same as the baby blues. According to the Diagnostic and Statistical Manual of Mental Disorders-5th edition (DSM-5), (American Psychiatric Association, 2013), peripartum onset of depression, also known as postpartum depression, is a type of depression that occurs during pregnancy or in the 4 weeks following pregnancy. Approximately 1 out of 8 women experience postpartum depression and symptoms can include feelings of sadness, sleeplessness, and difficulty bonding with the newborn.
Changing hormone levels are thought to be a factor in the occurrence of peripartum depression, however, risk factors include having depression previously, a family history of depression, being younger than 20, experiencing stress, and substance use. Peripartum-onset mood disorders, both depression and mania, can present with or without psychotic features. Hallucinations and delusions are associated with postpartum psychotic episodes and have included command hallucinations to kill the infant or delusions that the infant is possessed. Psychotic features occur in approximately 1 in 500 to 1 in 1,000 deliveries, and the risk is higher for women with prior postpartum mood episodes (American Psychiatric Association, 2013).
Postpartum anxiety is also a concern for many new mothers. According to Bregel (2017) because oxytocin, a bonding hormone, rises during pregnancy, brain areas related to empathy and anxiety are heightened. Consequently, the new mother is “hard-wired” to respond to and fend for her baby, which can lead to toxic levels of stress and anxiety. These can manifest as heightened alertness, intrusive and horrifying thoughts of something terrible happening to the infant, and physiological arousal. Just as for peripartum depression and postpartum psychosis, a new mother experiencing postpartum anxiety should seek assistance from a health care provider.[51]
Test Yourself:
- Children’s Development by Ana R. Leon is licensed under CC BY 4.0 ↵
- MacDorman MF, Declercq E. Trends and state variations in out-of-hospital births in the United States, 2004-2017. Birth. 2019 Jun;46(2):279-288. doi: 10.1111/birt.12411. Epub 2018 Dec 10. PMID: 30537156; PMCID: PMC6642827. Public Domain ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Changes in Home Births by Race and Hispanic Origin and State of Residence of the Mother: United States, 2019-2020 and 2020-2021 by Elizabeth C.W Gregory, M.P.H, Michelle J.K. Osterman, M.H.S, and Claudia P. Valenzuela, M.P.H.. National Vital Statistics Reports. ↵
- Changes in Home Births by Race and Hispanic Origin and State of Residence of the Mother: United States, 2019-2020 and 2020-2021 by Elizabeth C.W Gregory, M.P.H, Michelle J.K. Osterman, M.H.S, and Claudia P. Valenzuela, M.P.H.. National Vital Statistics Reports. ↵
- Children’s Development by Ana R. Leon is licensed under CC BY 4.0 (Modified by Maria Pagano). ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 (Modified by Maria Pagano) ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Machover, Ilana. (n.d.). The Alexander Technique in Natural Childbirth. Retrieved from https://www.alexandertechnique.com/articles/childbirth/. ↵
- Water Birth by Wikidoc is licensed under CC BY-SA 3.0 ↵
- Lotus Birth by Wikipedia is licensed under CC BY-SA 3.0 ↵
- Silent Birth by Wikipedia is licensed under CC BY-SA 3.0 ↵
- Image by liz.schrenk is licensed under CC BY-NC-ND 2.0 ↵
- 28.4 Maternal Changes During Pregnancy, Labor, and Birth by Lindsay M. Biga, Sierra Dawson, Amy Harwell, Robin Hopkins, Joel Kaufmann, Mike LeMaster, Philip Matern, Katie Morrison-Graham, Devon Quick, and Jon Runyeon is licensed under CC BY-NC-SA 4.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by OpenStax is licensed under CC BY 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by OpenStax is licensed under CC BY 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective (page 60) by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by U.S. Army Alaska is licensed under CC BY 2.0 ↵
- Maria Pagano licensed under CC BY SA 3.0 ↵
- Table and text adapted from Wikipedia and is licensed under CC BY SA 3.0 ↵
- Text adapted from Wikipedia and is licensed under CC BY SA 3.0 ↵
- ”Cervical Ripening in the Outpatient Setting” from Agency for Healthcare Research and Quality, U.S Department of Health and Human Services. No Author Attribution Found. Public Domain. ↵
- Mahdy H, Glowacki C, Eruo FU. Amniotomy. [Updated 2021 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470167/ . Licensed under CC BY 4.0 ↵
- Image by Tammra M is licensed under CC BY 2.0 ↵
- Image by Patricia Prudente on Unsplash ↵
- Lifespan Development: A Psychological Perspective (page 61) by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Children’s Development by Ana R. Leon is licensed under CC BY 4.0 ↵
- From Lumen Learning, Authored by: Florida State College at Jacksonville. License: CC BY 4.0 ↵
- Image by Event Medicine Group ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by the U.S. Air Force is in the public domain ↵
- Newborn Screening is in the public domain ; Newborn Screening Program (NBS) by the California Department of Public Health is in the public domain ↵
- Image is in the public domain ↵
- Image by Upsilon Andromedae is licensed under CC BY 2.0 ↵
- Children’s Development by Ana R. Leon is licensed under CC BY 4.0 ↵
- Mongolian Spot by Wiktionary is licensed under CC BY-SA 3.0 ↵
- Image by NNethala is licensed under CC BY-SA 3.0 ↵
- Infant by WikiDoc is licensed under CC BY-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective (pages 62-63) by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0; Stillbirth by Wikipedia by Wikipedia is licensed under CC BY-SA 3.0 ↵
- Photo by Jennifer Paris used with permission ↵
- Child Growth and Development: An Open Educational Resources Publication by College of the Canyons by Jennifer Paris, Antoinette Ricardo, and Dawn Richmond is licensed under CC BY 4.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0; Stillbirth by Wikipedia by Wikipedia is licensed under CC BY-SA 3.0 ↵
- Children’s Development by Ana R. Leon is licensed under CC BY 4.0 ↵
- Lifespan Development: A Psychological Perspective 2nd Edition by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0[48] Materials developed by Centers for Disease Control and Prevention, National Vital Statistics System, Compressed Mortality File. Use of this material, including any links to the materials on the CDC,ATSDR or HHS websites, does not imply endorsement by CDC, ATSDR, HHS or the United States Government. ↵
- Materials developed by Centers for Disease Control and Prevention, National Vital Statistics System, Compressed Mortality File. Use of this material, including any links to the materials on the CDC,ATSDR or HHS websites, does not imply endorsement by CDC, ATSDR, HHS or the United States Government. ↵
- Lifespan Development: A Psychological Perspective 2nd Edition by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0[51] Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
a method by which an expectant mother is prepared for childbirth by education, psychological and physical conditioning, and breathing exercises.
emphasizes that birth is a natural process: mothers are encouraged to trust their body and focus on diet and exercise throughout pregnancy; and it teaches couples to manage labor through deep breathing and the support of a partner or labor coach.
a method of childbirth designed to reduce trauma for the newborn especially by avoiding the use of forceps and bright lights in the delivery room and by giving the newborn a warm bath
a technique of delivery called natural childbirth that minimized the surgical and anesthetic aspects of delivery and concentrated upon the mother's conscious effort to give birth to her child.
a technique for sitting, standing and moving with safety, efficiency, and ease. Anyone, including a pregnant woman, can learn to release muscular tension to increase breathing capacity and restore the body's original poise and proper posture.
technique where mom is submerged in water, usually in a stationary or inflatable tub, and you'll birth your baby in the water.
practice of birthing the baby and placenta, and leaving the two attached until the cord falls off on its own. Anecdotally, this can take 3 to 10 days,
see Lotus birth; decision to leave your baby’s umbilical cord attached after
they are born. The umbilical cord remains attached to the placenta until it dries
and falls off by itself.
everyone attending the birth refrains from spoken words as much as possible" doctors and nurses, shouts to 'PUSH, PUSH' and loud or laughing remarks to 'encourage' are avoided
a small amount of blood and mucus is released from the vagina. A bloody show occurs because the cervix starts to soften and thin (efface) and widen (dilate) in preparation for labor.
a collection of mucus that forms in the cervical canal in early pregnancy that prevents bacteria or infection from entering your uterus and reaching your baby. As the cervix prepares for labor, you lose the mucus plug. This is a normal and common symptom in late pregnancy.
The cervical canal passes through the cervix and allows blood from a menstrual period and a fetus to pass from the womb into the vagina.
the major endocrine gland. A pea-sized body attached to the base of the brain, the pituitary is important in controlling growth and development and the functioning of the other endocrine glands.
a hormone released by the pituitary gland that causes increased contraction of the uterus during labor and stimulates the ejection of milk into the ducts of the breasts.
any of a group of compounds with varying hormone-like effects, notably the promotion of uterine contractions.
surrounds the fetus during pregnancy and is a thin tissue composed of two layers, the chorion and the amnion.
The lower, narrow end of the uterus that forms a canal between the uterus and vagina.
occurs when you begin to feel persistent contractions. These contractions become stronger, more regular and more frequent over time. They cause the cervix to open (dilate) and soften as well as shorten and thin (efface) to allow your baby to move into the birth canal.
Also see Braxton Hicks contractions; irregular uterine contractions that are normal and might start to occur from fourth month of pregnancy.
see also false labor; tightening in one's abdomen that comes and goes. Contractions of the uterus in preparation for giving birth, which may tone the muscles of the uterus and may also help prepare the cervix for birth.
the fluid-filled sac that contains and protects a fetus in the womb.
cervix is fully dilated and ready for childbirth. This stage is the most work because your provider wants you to start pushing your baby out. This stage can be as short as 20 minutes or as long as a few hours. It may be longer for first-time moms or if you've had an epidural.
a surgical cut made at the opening of the vagina during childbirth, to aid a difficult delivery and prevent rupture of tissues.
the time between the delivery of the baby and the expulsion of the placenta. The duration of the third stage is ~6-30 minutes
anesthesia produced by the injection of an anesthetic into the lumbar area of the spine in the space between the spinal cord and the dura, which eliminates sensation from the point of insertion downward, used especially in childbirth.
An injection of an anesthetic drug into the space between the wall of the spinal canal and the covering of the spinal cord.
In obstetric patients, regional analgesia refers to partial or complete loss of pain sensation below the T8 to T10 spinal level.
Also called a C-section; a surgical operation for delivering a child by cutting through the wall of the mother's abdomen.
a large instrument with broad pincers, used to encircle a baby's head and assist in birth.
the application of reduced pressure to extract something, particularly to assist childbirth or as a method of abortion, or as a technique for removing components of a chemical mixture.
an injection into the pelvic region that can provide temporary pain relief.
anesthesia that affects the whole body and usually induces a loss of consciousness.
childbirth with minimal medical or technological intervention, usually involving special breathing and relaxation techniques.
prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
see induction of labor; when your health care provider gives you medicine or uses other methods to make labor start.
the treatment of a disorder or disease with medication.
a synthetic form of oxytocin, used to induce labor.
a system used by medical professionals to decide how likely it is that you will go into labor soon.
the thinning of the cervix during labor. It's also described as a softening, shortening, or ripening.
basin-shaped complex of bones that connects the trunk and the legs, supports and balances the trunk, and contains and supports the intestines, the urinary bladder, and the internal sex organs.
when the cervix changes from being closed and firm to soft and thin
the cervix opens (dilates) and thins out (effaces) to allow the baby to move into the birth canal
a flexible tube inserted through a narrow opening into a body cavity
a type of catheter incorporating a small balloon which may be introduced into a canal, duct, or blood vessel and then inflated in order to clear an obstruction or dilate a narrowed region.
also known as artificial rupture of membranes (AROM) or as "breaking the water," is the intentional rupture of the amniotic sac.
scoring system that provides a standardized assessment for infants after delivery. The Apgar score comprises five components: 1) color, 2) heart rate, 3) reflexes, 4) muscle tone, and 5) respiration, each of which is given a score of 0, 1, or 2.
an instrument designed to assess the neurological and behavioral functioning of newborn and very young infant. It assesses the infants' ability to tune out stimuli, to respond to visual and auditory stimuli, motor functioning and reflexes.
A simple procedure in which a newborn baby's heel is pricked and then a small amount of the blood is collected, usually with a narrow-gauge ("capillary") glass tube or a filter paper.
fine, soft hair, especially that which covers the body and limbs of a human fetus or newborn.
a greasy deposit covering the skin of a baby at birth.
a kind of birthmark that is flat, blue, or blue-gray.
an absence of oxygen.
A term used to describe an infant born weighing 5.5 pounds (2500 grams) or less.
babies who are born weighing less than 1,500 grams (3 pounds, 4 ounces)
when a baby is born too early, before 37 weeks of pregnancy have been completed.
A substance that reduces inflammation (redness, swelling, and pain) in the body.
occurs in babies born early (premature) whose lungs are not fully developed.
a medical condition with yellowing of the skin or whites of the eyes, arising from excess of the pigment bilirubin and typically caused by obstruction of the bile duct, by liver disease, or by excessive breakdown of red blood cells.
nursery in a hospital that provides around-the-clock care to sick or premature babies.
a baby who is smaller than the usual amount for the number of weeks of pregnancy; babies usually having birthweights below the 10th percentile for babies of the same gestational age
any baby born after 42 weeks gestation or 294 days past the first day of the mother's last menstrual period.
the death or loss of a baby before or during delivery.
a woman employed to breast-feed another woman's child.
lack of proper nutrition, caused by not having enough to eat, not eating enough of the right things, or being unable to use the food that one does eat.
one of the most common severe nutritional disorders affecting children of developing countries.
accustom (an infant or other young mammal) to food other than its mother's milk.
a form of malnutrition caused by protein deficiency in the diet, typically affecting young children in the tropics.
iron-deficiency anemia caused by consistent consumption of milk in amounts greater than 1 quart daily.
sleeping over more than two sleeping periods each day. These periods could be quick nap breaks throughout the day balanced with a reduced time asleep during the night.
Also called REM sleep; a jerky motion of a person's eyes occurring in REM sleep; during REM sleep, a person's brain activity, breathing, heart rate, and blood pressure increase, and the eyes move rapidly while closed.
a term used to describe the sudden and unexpected death of a baby less than 1 year old in which the cause was not obvious before investigation. These deaths often happen during sleep.
the death of a seemingly healthy baby in its sleep, due to an apparent spontaneous cessation of breathing.
occurs when something limits a baby's breathing, like when soft bedding or blankets are against their face or when a baby gets trapped between two objects, such as a mattress and wall.
depression suffered by a mother following childbirth, typically arising from the combination of hormonal changes, psychological adjustment to motherhood, and fatigue.
also called postpartum depression; refers to depression occurring during pregnancy or after childbirth.
distressing feelings that occur during pregnancy (perinatal) and throughout the first year after pregnancy (postpartum).
a serious mental health illness that can affect someone soon after having a baby. Symptoms include severe agitation, confusion, feelings of hopelessness and shame, insomnia, paranoia, delusions or hallucinations, hyperactivity, rapid speech or mania.
excessive worrying that occurs after childbirth or adoption.