4 Prenatal Development
Learning Objectives
After reading Chapter 4 , you should be better equipped to:
- Describe changes that occur within each of the three periods of prenatal development
- Recognize the risks to prenatal development posed by exposure to teratogens.
- Evaluate different types of prenatal assessment.
- Describe complications associated with pregnancy
- Evaluate infertility options
Prenatal Development
The process by which an organism develops from a single-celled zygote to a multi-cellular organism is complex and well regulated. The regulation occurs through signaling between cells and tissues and responses in the form of differential gene expression. This chain of prenatal development is divided into three periods, the germinal period or zygote period, the embryonic period, and the fetal period.
From Conception to Zygote
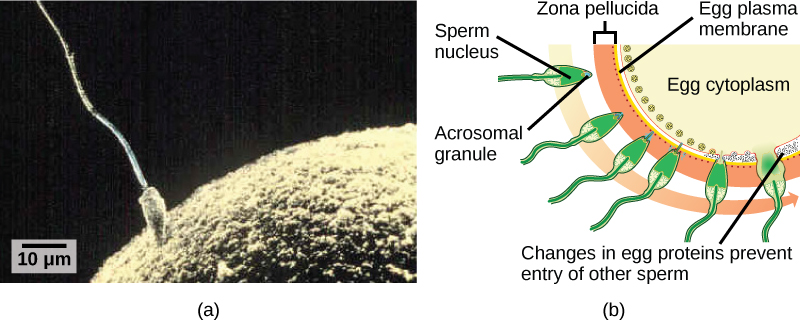
The germinal or zygote period (about 14 days in length) lasts from conception to implantation of the fertilized egg in the lining of the uterus. At ejaculation millions of sperm are released into the vagina, but only a few reach the egg and typically only one fertilizes the egg. Once a single sperm has entered the wall of the egg, the wall becomes hard and prevents other sperm from entering. After the sperm has entered the egg, the tail of the sperm breaks off and the head of the sperm, containing the genetic information from the father, unites with the nucleus of the egg. It is typically fertilized in the top section of the fallopian tube and continues its journey to the uterus. As a result, a new cell is formed. This cell, containing the combined genetic information from both parents, is referred to as a zygote.[1]
To ensure that the offspring has only one complete diploid set of chromosomes, only one sperm must fuse with one egg. In all mammals, a layer called the zona pellucida protects the egg. At the tip of the head of a sperm cell is a structure like a lysosome called the acrosome, which contains enzymes. When a sperm binds to the zona pellucida, a series of events, called the acrosomal reactions, take place. These reactions, involving enzymes from the acrosome, allow the sperm plasma membrane to fuse with the egg plasma membrane and permit the sperm nucleus to transfer into the ovum. The nuclear membranes of the egg and sperm break down and the two haploid nuclei fuse to form a diploid nucleus or genome.
Sperm and Ovum at Conception[2]
During this time, the organism begins cell division through mitosis, however this is a fragile process and fewer than one half of all zygotes survive beyond the first two weeks (Hall, 2004). Some of the reasons for this include the egg and sperm do not join properly, thus their genetic material does not combine, there is too little or damaged genetic material, the zygote does not replicate, or the blastocyst does not implant into the uterine wall. The failure rate is higher for in vitro conceptions. The figure below illustrates the journey of the ova from its release to its fertilization, cell duplication, and implantation into the uterine lining.[3]
Fertilized Egg Traveling Through the Fallopian Tube[4]
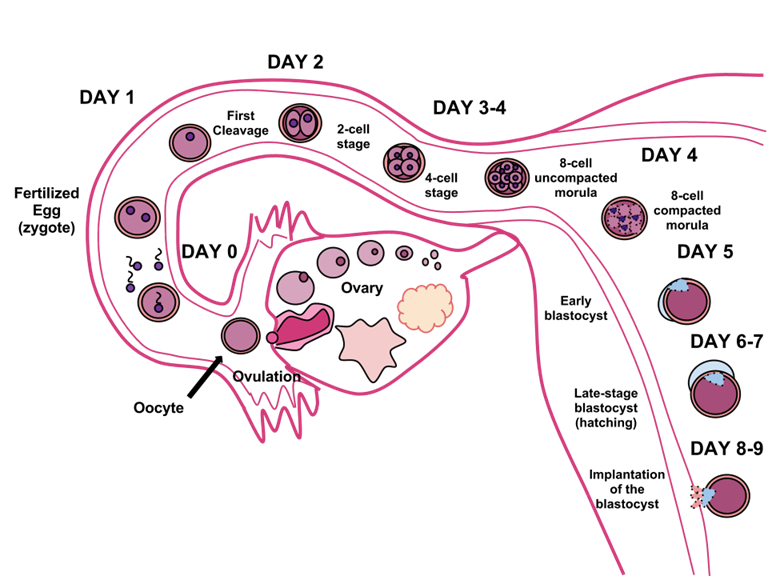
After five days of mitosis there are 100 cells, and this mass of cells is now called a blastocyst. The blastocyst consists of both an inner and outer group of cells. The inner group of cells, or inner cell mass will become the embryo, The outer group of cells, the trophoblast, secretes enzymes that allow implantation of the blastocyst into the uterine wall, contributes to the development of the placenta, and becomes the support system which nourishes the developing organism. This stage ends when the blastocyst fully implants into the uterine wall (U.S. National Library of Medicine, 2015).[5]
Layers of a Blastocyst
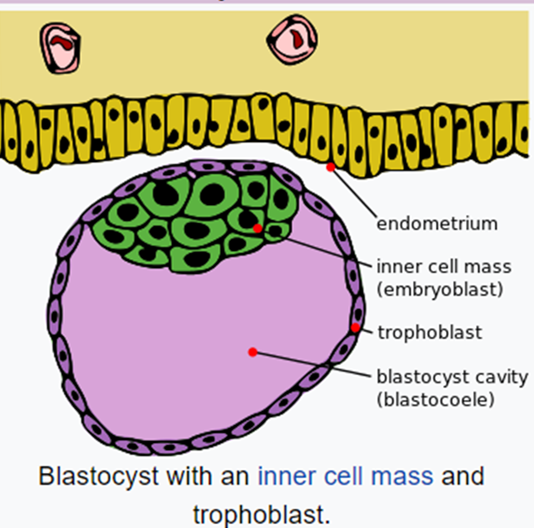
Image of the blastocyst at 6 days which shows the inner cell mass, which will become the fetus, the trophoblast which will form the placenta, and the blastocoel, a fluid-filled cavity. The endometrium is the lining of the uterus where the embryo will implant. [6]
Test Yourself: Each of the areas below with a “?” indicates an area of the blastocyst. Can you determine which of each area will develop into what area of the organism? Hover over the “?” to get the correct answer. Note that there is no scoring for this review.
Test Yourself
The Embryonic Period
Starting the third week, the blastocyst has implanted in the uterine wall. Upon implantation this multi-cellular organism is called an embryo. It is during this stage of embryonic development that the body plan is formulated. The cells in the blastocyst rearrange themselves spatially to form three layers of cells through a process called gastrulation. During gastrulation, the blastocyst folds upon itself to form three layers of cells. Each of these layers is called a germ layer and each germ layer differentiates into different organ systems.
The three germs layers, shown below, are the endoderm, the ectoderm, and the mesoderm. The ectoderm gives rise to the nervous system and the epidermis. The mesoderm gives rise to the muscle cells and connective tissue in the body. The endoderm gives rise to columnar cells found in the digestive system and many internal organs.[7]
The Endoderm, Mesoderm, and Ectoderm Layers[8]
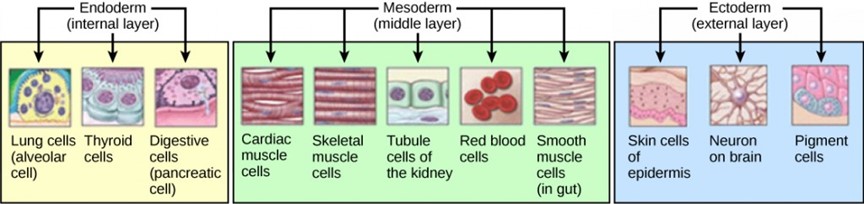
Through gastrulation, the formation of the three germ layers give rise during further development to the different organs in the animal body. This process is called organogenesis. Organs develop from the germ layers through the process of differentiation. During differentiation, the embryonic stem cells express specific sets of genes that will determine their ultimate cell type. For example, some cells in the ectoderm will express the genes specific to skin cells. As a result, these cells will take on the shape and characteristics of epidermal cells. The process of differentiation is regulated by location-specific chemical signals from the cell’s embryonic environment that sets in play a cascade of events that regulates gene expression.[9]
During the embryonic period, cells continue to differentiate. Growth during prenatal development occurs in two major directions: from head to tail called cephalocaudal development and from the midline outward referred to as proximodistal development. This means that those structures nearest the head develop before those nearest the feet and those structures nearest the torso develop before those away from the center of the body (such as hands and fingers). You will see that this pattern continues after birth.
The head develops in the fourth week and the precursor to the heart begins to pulse. In the early stages of the embryonic period, gills and a tail are apparent. However, by the end of this stage they disappear and the organism takes on a more human appearance.
Human Embryo – (Approximately 8 weeks estimated gestational age) [10]

About 20 percent of organisms fail during the embryonic period, usually due to gross chromosomal abnormalities, often before the mother even knows that she is pregnant. It is during this stage that the major structures of the body are taking form, making the embryonic period the time when the organism is most vulnerable to the greatest amount of damage if exposed to harmful substances. Prospective mothers are not often aware of the risks they introduce to the developing embryo during this time. The embryo is approximately 1 inch in length and weighs about 4 grams at the end of eight weeks. The embryo can move and respond to touch at this time.
Test Yourself
The Fetal Period
From the ninth week until birth (which is forty weeks for a full-term pregnancy), the organism is referred to as a fetus. During this stage, the major structures are continuing to develop. By the third month, the fetus has all its body parts including external genitalia. The fetus is about 3 inches long and weighs about 28 grams. In the following weeks, the fetus will develop hair, nails, teeth and the excretory and digestive systems will continue to develop. [11]
A Fetus Sucking its Thumb[12]

During the 4th – 6th months, the eyes become more sensitive to light and hearing develops. The respiratory system continues to develop, and reflexes such as sucking, swallowing, and hiccupping, develop during the 5th month. Cycles of sleep and wakefulness are also present as well. The first chance of survival outside the womb, known as the age of viability, is reached at about 24 weeks (Morgan, Goldenberg, & Schulkin, 2008). Many practitioners hesitate to resuscitate before 24 weeks. Most of the neurons in the brain have developed by 24 weeks, although they are still rudimentary, and the glial or nurse cells that support neurons continue to grow. At 24 weeks the fetus can feel pain (Royal College of Obstetricians and Gynecologists, 1997).
Between the 7th – 9th months, the fetus is primarily preparing for birth. It is exercising its muscles and its lungs begin to expand and contract. The fetus gains about 5 pounds and 7 inches during this last trimester of pregnancy, and during the 8th month a layer of fat develops under the skin. This layer of fat serves as insulation and helps the baby regulate body temperature after birth.
At around 36 weeks the fetus is almost ready for birth. It weighs about 6 pounds and is about 18.5 inches long. By week 37 all of the fetus’s organ systems are developed enough that it could survive outside the mother’s uterus without many of the risks associated with premature birth. The fetus continues to gain weight and grow in length until approximately 40 weeks. By then the fetus has very little room to move around and birth becomes imminent. The progression through the fetal and embryonic stages can be found in the following figure.[13]
Prenatal Development of the Fetus[14]

Test Yourself
| Monozygotic and Dizygotic Twins | |
| Monozygotic or identical twins occur when a fertilized egg splits apart in the first two weeks of development. The result is the creation of two separate, but genetically identical offspring. That is, they possess the same genotype and often the same phenotype. About one-third of twins are monozygotic twins.
Sometimes, however, two eggs or ova are released and fertilized by two separate sperm. The result is dizygotic or fraternal twins. These two individuals share the same amount of genetic material as would any two children from the same mother and father, which is 50%. In other words, they possess a different genotype and phenotype.
Older mothers are more likely to have dizygotic twins than are younger mothers, and couples who use fertility drugs are also more likely to give birth to dizygotic twins.[15]
|
|
| Monozygotic Twins[16] | |

Dizygotic Twins[17]
|
|
Prenatal Brain Development
Prenatal brain development begins in the third gestational week with the differentiation of stem cells, which can produce all the different cells that make up the brain (Stiles & Jernigan, 2010). The location of these stem cells in the embryo is referred to as the neural plate. [18] The formation and folding of the neural plate is the first step in primary neurulation, which is then followed by the refinement and growth of neural plate cells. The third step of primary neurulation does not involve the neural plate per se, but rather the edges of the neural plate, which come together, turning the plate into the start of the neural tube. With the neural plate having folded into a tube, the neural folds come together to complete the fusion of the neural tube. This process is illustrated in the figure below, where the neural plate is shown in purple. The lime green marks the edges of the neural plate, which become the neural folds, that are involved in the folding of the plate to create the neural tube. The figure below demonstrates the development of the neural plate into the neural tube, which is where the neural crest cells are derived from as well.[19]
Development of the Neural Tube
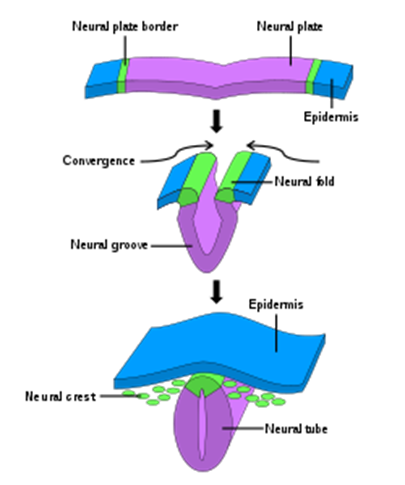
By the end of the third week, two ridges appear along the neural plate first forming the neural groove and then the neural tube. The open region in the center of the neural tube forms the brain’s ventricles and spinal canal. By the end of the embryonic period, or week eight, the neural tube has further differentiated into the forebrain, midbrain, and hindbrain. [20]
Test Yourself: Answer the following three, true/false questions to test your knowledge of primary neurulation. Click on the “>” to move to the next question.
Brain development during the fetal period involves neuron production, migration, and differentiation. From the early fetal period until mid-gestation, most of the 85 billion neurons have been generated and many have already migrated to their brain positions. Neurogenesis, or the formation of neurons, is largely completed after five months of gestation. One exception is in the hippocampus, which continues to develop neurons throughout life. Neurons that form the neocortex, or the layer of cells that lie on the surface of the brain, migrate to their location in an orderly way. Neural migration is mostly completed in the cerebral cortex by 24 weeks (Poduri & Volpe, 2018). Once in position, neurons begin to produce dendrites and axons that begin to form the neural networks responsible for information processing. Regions of the brain that contain the cell bodies are referred to as the gray matter because they look gray in appearance. The axons that form the neural pathways make up the white matter because they are covered in myelin, a fatty substance that is white in appearance. Myelin aids in both the insulation and efficiency of neural transmission. Although cell differentiation is complete at birth, the growth of dendrites, axons, and synapses continue for years.[21]
Teratogens
Good prenatal care is essential to protect against maternal and fetal/infant mortality and birth complications. The embryo and fetus are most at risk for some of the most severe problems during the first three months of development. Unfortunately, this is a time at which many mothers are unaware that they are pregnant. Today, we know many of the factors that can jeopardize the health of the developing child. The study of factors that contribute to birth defects is called teratology, and the environmental factors that can contribute to birth defects are called teratogens. Teratogens include some maternal diseases, pollutants, drugs, and alcohol.
There are several considerations in determining the type and amount of damage that might result from exposure to a particular teratogen (Berger, 2005). These include:
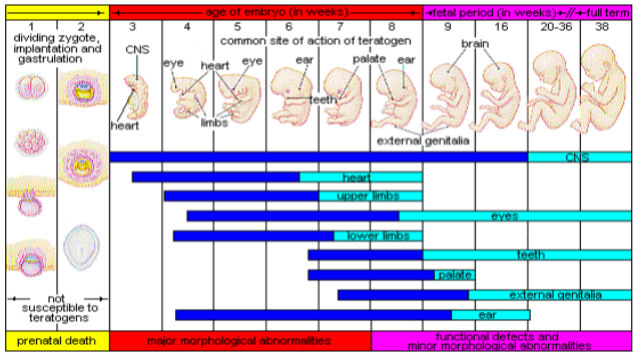
- The timing of the exposure: Structures in the body are vulnerable to the most severe damage when they are forming. If a substance is introduced during a particular structure’s critical period (time of development), the damage to that structure may be greater. For example, the ears and arms reach their critical periods at about 6 weeks after conception. If a mother exposes the embryo to certain substances during this period, the arms and ears may be malformed. (see figure below)
- The amount of exposure: Some substances are not harmful unless the amounts reach a certain level. The critical level depends in part on the size and metabolism of the mother.
- The number of teratogens: Fetuses exposed to multiple teratogens typically have more problems than those exposed to only one.
- Genetics: Genetic makeup also plays a role on the impact a particular teratogen might have on the child. This is suggested by fraternal twins exposed to the same prenatal environment, but they do not experience the same teratogenic effects. The genetic makeup of the mother can also have an effect; some mothers may be more resistant to teratogenic effects than others.
- Being male or female: Males are more likely to experience damage due to teratogens than are females. It is believed that the Y chromosome, which contains fewer genes than the X, may have an impact.[22]
Critical Periods of Prenatal Development[23]
There are four categories of teratogens:
- Drugs and chemicals: When pregnant females ingest or absorb these, they may cause a variety of different effects based on specific agent, amount of exposure, and timing. This category includes radiation, heavy metals (including lead), insecticides and herbicides, prescription and over the counter drugs, illicit and recreational drugs, alcohol, cigarettes, nicotine, caffeine, and even some vitamins.
- Infections: Different maternal infections, including rubella virus, herpes simplex virus, and syphilis can cause congenital abnormalities in fetuses.
- Physical teratogens: In utero exposure to radiation, typically in the forms of X-rays can lead to growth restrictions, (smaller head circumference at birth and small eyes), malformations and impaired brain functioning. Saunas, hot tubs, or infections that raise a pregnant woman’s body temperature to 102 degrees Fahrenheit or higher are associated with neural tube defects, spontaneous abortions, and various cardiovascular abnormalities. to a fetus from radiation exposure depend largely on the radiation dose.
- Metabolic conditions affecting pregnant females: Metabolic conditions are abnormalities in the chemical process of producing energy from food, and thereby affect the development and function of the body. If a pregnant woman is malnourished, then her fetus likely lacks the nutrients essential for its development. These include malnutrition, diabetes, and thyroid disorders.[24]
1. Drugs and Chemicals as Teratogens
Alcohol
One of the most common teratogens is alcohol, and because half of all pregnancies in the United States are unplanned, it is recommended that women of child-bearing age take great caution against drinking alcohol when not using birth control or when pregnant (CDC, 2005). Alcohol use during pregnancy is the leading preventable cause of intellectual disabilities in children in the United States (Maier & West, 2001). Alcohol consumption at any point during pregnancy, but particularly during the second month of prenatal development, may lead to neurocognitive and behavioral difficulties that can last a lifetime.[25]
Fetal Alcohol Spectrum Disorders (FASD) is a collection of developmental disorders affecting offspring that result from a woman drinking alcohol while she is pregnant. These disorders range from mild learning disabilities, to memory and attention deficits, to birth defects, to developmental delays, to serious behavior disorders, to sudden infant death syndrome. Drinking during pregnancy is the leading known cause of preventable birth defects in the Western world. To prevent these birth defects, the answer is simple. A woman should not drink alcohol while she is pregnant or even if she might become pregnant because…
- There is no known amount of alcohol that is safe during pregnancy.
- There is no known time during pregnancy that is safe to drink.
- And, there is no drink that contains alcohol that is safe.
Fetal Alcohol Spectrum Disorders are found across all social, economic, and racial groups. This spectrum of disorders includes the following:
- Fetal Alcohol Syndrome (FAS)
- Includes a pattern of facial abnormalities, growth retardation, insufficient brain growth, and distinct behavioral and cognitive (thinking abilities) abnormalities
- Alcohol-Related Birth Defects (ARBD)
- Includes minor facial abnormalities, structural or functional defects of organs (heart, skeleton, kidneys, eyes, or ears), and cognitive and behavioral abnormalities
- Alcohol-Related Neurodevelopmental Disorders (ARND)
- Consists of insufficient brain growth and distinct behavioral and cognitive abnormalities
Clearly, there is a vast spectrum of abnormalities associated with prenatal alcohol exposure. The range of these abnormalities is dependent on many factors, including the amount of alcohol consumed, the developmental stage of pregnancy when exposed, and the mothers’ pattern of drinking. Other factors that affect the severity of FASD include the nutritional status of the mother, any of drugs of abuse she may be taking during pregnancy, and her genetics.
Physical features associated with Fetal Alcohol Spectrum Disorders
The physical features resulting from exposure of the fetus to alcohol have been well-described. Several are quite typical of children with FAS and ARBD. These include, 1) a specific set of facial abnormalities (discussed below), 2) other organ structural defects, 3) prenatal and/or postnatal growth deficiency (below the 10th percentile for height or weight), and 4) a reduced head circumference. These features can occur in any combination in any child (although not all) exposed to alcohol prenatally. An example of the types of facial abnormalities is shown in the figure below.
Facial Abnormalities associated with FAS and ARBD
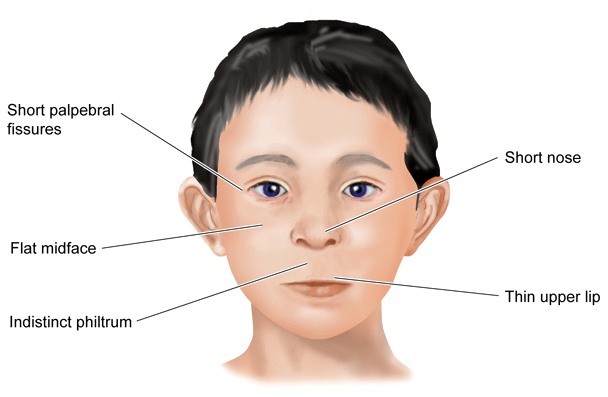
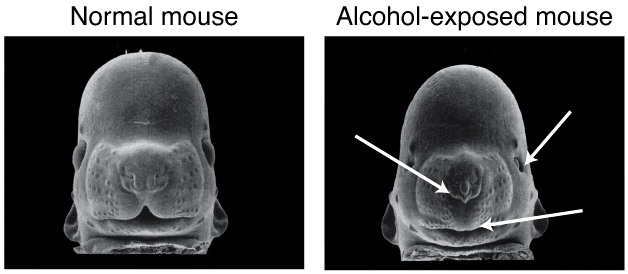
Scientists have studied how alcohol causes developmental abnormalities in facial structure in animal models. For example, look at a picture of the faces of a normal mouse fetus and a mouse fetus that was exposed to a high dose of alcohol by its mother. The facial abnormalities are very similar to humans with FAS or ARBD.
While very evident during childhood, many of these facial abnormalities tend to become less apparent with age, and adults with FAS may no longer show the classic facial characteristics. Some of the structural features can cause functional problems as well. For example, there can be reduced vision due to retinal malformations.
Not all people exposed to alcohol during pregnancy show the facial abnormalities. In the picture below, can you tell who has FASD?
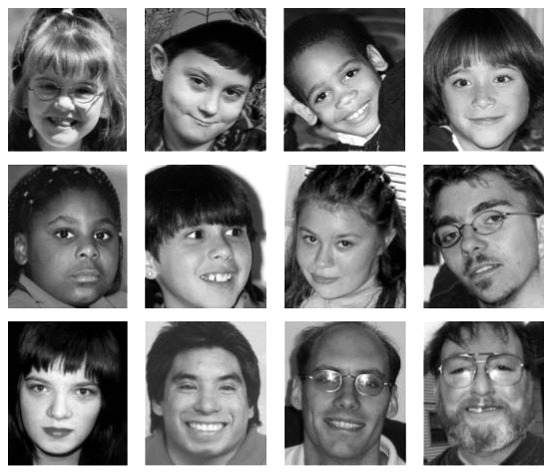
If you answered that all of them have FASD, you are right. Some people have very prominent facial abnormalities, and others look perfectly normal. However, they all still suffer the neurocognitive and behavioral abnormalities discussed below.
Not all physical abnormalities caused by prenatal alcohol can be seen with the “naked eye”. For example, some organs inside the body fail to develop normally. And our most precious organ, the brain, clearly shows structural abnormalities with the help of technologies such as magnetic resonance imaging (MRI).
Neurocognitive and behavioral abnormalities associated with FASD
In addition to the structural problems, the effects of alcohol on a fetus can produce a host of other symptoms throughout childhood and adulthood, notably neurocognitive or behavioral problems and learning disabilities. While not all children exposed to alcohol prenatally exhibit these symptoms, the most common ones are listed below.
Neurocognitive and behavioral problems include:
- Average low IQ (can range from severe mental retardation to normal)
- Poor executive functioning
- Lack of social and communication skills
- Lack of appropriate initiative
- Poor judgment
- Failure to consider consequences of actions
- Poor concentration and attention
- Social withdrawal
- Poor impulse control
- Intermittent anxiety
- Stubbornness
Children who have FASD exhibit some combination of these cognitive and behavioral problems, regardless of when the mother drinks alcohol. Often, these children are mislabeled with other disorders such as Attention Deficit Hyperactivity Disorder (ADHD) because of some of the similarities in their behavioral problems.[26]
Tobacco
According to the Centers for Disease Control and Prevention (Drake, Driscoll, and Mathews 2016) approximately 7.2% of women who gave birth smoked cigarettes during pregnancy. When a pregnant woman smokes the fetus is exposed to dangerous chemicals including nicotine, carbon monoxide and tar, which lessen the amount of oxygen available to the fetus. Oxygen is important for overall growth and development. Tobacco use during pregnancy has been associated with low birth weight, ectopic pregnancy (fertilized egg implants itself outside of the uterus), placenta previa (placenta lies low in the uterus and covers all or part of the cervix), placenta abruption (placenta separates prematurely from the uterine wall), preterm delivery, stillbirth, fetal growth restriction, sudden infant death syndrome (SIDS), birth defects, learning disabilities, and early puberty in girls (Center for Disease Control, 2015d).
A woman being exposed to secondhand smoke during pregnancy has also been linked to low-birth weight infants. In addition, exposure to thirdhand smoke, or toxins from tobacco smoke that linger on clothing, furniture, and in locations where smoking has occurred, results in a negative impact on infants’ lung development. Rehan, Sakurai, and Torday (2011) found that prenatal exposure to thirdhand smoke played a greater role in altered lung functioning in children than exposure postnatally.
Prescription/Over-the-counter Drugs: About 70% of pregnant women take at least one prescription drug (March of Dimes, 2016e). A woman should not be taking any prescription drug during pregnancy unless it was prescribed by a health care provider who knows she is pregnant. Some prescription drugs can cause birth defects, problems in overall health, and development of the fetus. Over-the-counter drugs are also a concern during the prenatal period because they may cause certain health problems. For example, the pain reliever ibuprofen can cause serious blood flow problems to the fetus during the last three months.
Illicit Drugs
Common illicit drugs include cocaine, ecstasy and other club drugs, heroin, marijuana, and prescription drugs that are abused. It is difficult to completely determine the effects of a particular illicit drug on a developing child because most mothers who use, use more than one substance and have other unhealthy behaviors. These include smoking, drinking alcohol, not eating healthy meals, and being more likely to get a sexually transmitted disease. However, several problems seem clear. The use of cocaine is connected with low birth weight, stillbirths and spontaneous abortion. Heavy marijuana use is associated with problems in brain development (March of Dimes, 2016c). If a baby’s mother used an addictive drug during pregnancy that baby can get addicted to the drug before birth and go through drug withdrawal after birth, also known as Neonatal abstinence syndrome (March of Dimes, 2015d). Other complications of illicit drug use include premature birth, smaller than normal head size, birth defects, heart defects, and infections. Additionally, babies born to mothers who use drugs may have problems later in life, including learning and behavior difficulties, slower than normal growth, and die from sudden infant death syndrome. Children of substance abusing parents are also considered at high risk for a range of biological, developmental, academic, and behavioral problems, including developing substance abuse problems of their own (Conners, et al., 2003).
Women who use drugs or alcohol during pregnancy can cause serious lifelong harm to their child. Some people have advocated mandatory screenings for women who are pregnant and have a history of drug abuse, and if the women continue using, to arrest, prosecute, and incarcerate them (Figdor & Kaeser, 1998). This policy was tried in Charleston, South Carolina 20 years ago. The policy was called the Interagency Policy on Management of Substance Abuse During Pregnancy and had disastrous results: The Interagency Policy applied to patients attending the obstetrics clinic at MUSC, which primarily serves patients who are indigent or on Medicaid. It did not apply to private obstetrical patients. The policy required patient education about the harmful effects of substance abuse during pregnancy. A statement also warned patients that protection of unborn and newborn children from the harms of illegal drug abuse could involve the Charleston police, the Solicitor of the Ninth Judicial Court, and the Protective Services Division of the Department of Social Services (DSS). (Jos, Marshall, & Perlmutter, 1995, pp. 120–121) This policy seemed to deter women from seeking prenatal care, deterred them from seeking other social services, and was applied solely to low-income women, resulting in lawsuits. The program was canceled after 5 years, during which 42 women were arrested. A federal agency later determined that the program involved human experimentation without the approval and oversight of an institutional review board (IRB). In July 2014, Tennessee enacted a law that allows women who illegally use a narcotic drug while pregnant to be prosecuted for assault if her infant is harmed or addicted to the drug (National Public Radio, 2015). According to the National Public Radio report, a baby is born dependent on a drug every 30 minutes in Tennessee, which is a rate three times higher than the national average. However, since the law took effect the number of babies born having drug withdrawal symptoms has not diminished. Critics contend that the criminal justice system should not be involved in what is considered a healthcare problem. What do you think? Is the issue of mothers using illicit drugs more of a legal or medical concern?
Sample Listing of Drugs Which Have Possible Teratogenetic Effects
| Teratogen | Potential Effects |
| Caffeine | Moderate amounts of caffeine (200 mg or around 12 ounces of coffee) appear to be safe during pregnancy. Some studies have shown a link between higher amounts of caffeine and miscarriage and preterm birth.[27] |
| Tobacco | Tobacco use has been associated with low birth weight, placenta previa, preterm delivery, fetal growth restriction, sudden infant death syndrome, cleft lip or palate, and later health problems (such as high blood pressure and diabetes).[28] |
| Alcohol | There is no safe amount of alcohol a woman can drink while pregnant. Alcohol can slow down the baby’s growth, affect the baby’s brain, and cause birth defects, and may results in fetal alcohol spectrum disorder (FASD). The effects can be mild to severe. Children born with a severe form of FASD can have abnormal facial features, severe learning disabilities, behavioral problems, and other problems.[29] |
| Cocaine | Cocaine use has connected with low birth weight, stillbirths, spontaneous abortion, placental abruption, premature birth, miscarriage, and neonatal abstinence syndrome (fetal addiction leads the newborn to experiences withdrawal).[30] |
| Marijuana | No amount of marijuana has been proven safe to use during pregnancy. Heavy use has been associated with brain damage, premature birth, and stillbirth.[31] |
| Heroin | Using heroin during pregnancy can cause birth defects, placental abruption, premature birth, low birthweight, neonatal abstinence syndrome, still birth, and sudden infant death syndrome.[32] |
| Over-the-Counter (OTC) medication | Some OTC medications are safe to use during pregnancy and others may cause health problems during pregnancy. Pregnant women should consult their health care provider before using OTC medications.[33] |
| Prescription drugs | Some prescription drugs can cause birth defects that change the shape or function of one or more parts of the body that can affect overall health. Pregnant women should consult their health care provider before discontinuing or starting new medications.[34] |
| Herbal or dietary supplements | Except for some vitamins, little is known about using herbal or dietary supplements while pregnant. Most often there are no good studies to show if the herb can cause harm to you or your baby. Also, some herbs that are safe when used in small amounts as food might be harmful when used in large amounts as medicines.[35] |
Chemical Pollutants
There are more than 83,000 chemicals used in the United States with little information on the effects of them during pregnancy (March of Dimes, 2016b).
- Lead: An environmental pollutant of significant concern is lead poisoning, which has been linked to fertility problems, high blood pressure, low birth weight, prematurity, miscarriage, and slowed neurological development. Grossman and Slutsky (2017) found that babies born in Flint Michigan, an area identified with high lead levels in the drinking water, were premature, weighed less than average, and gained less weight than expected.
- Pesticides: The chemicals in certain pesticides are also potentially damaging and may lead to birth defects, learning problems, low birth weight, miscarriage, and premature birth (March of Dimes, 2014).
- Bisphenol A: Prenatal exposure to bisphenol A (BPA), a chemical commonly used in plastics and food and beverage containers, may disrupt the action of certain genes contributing to certain birth defects (March of Dimes, 2016b).
- Radiation: If a mother is exposed to radiation, it can get into the bloodstream and pass through the umbilical cord to the baby. Radiation can also build up in body areas close to the uterus, such as the bladder. Exposure to radiation can slow the baby’s growth, cause birth defects, affect brain development, cause cancer, and result in a miscarriage.
- Mercury: Mercury, a heavy metal, can cause brain damage and affect the baby’s hearing and vision. This is why women are cautioned about the amount and type of fish they consume during pregnancy.
Chemical Pollutants as Teratogens
| Teratogen | Potential Effects |
| Lead | Exposure to high levels of lead before and during pregnancy can lead to high blood pressure, problems with fetal brain and nervous system development, premature birth, low birthweight, and miscarriage.[36] |
| Mercury | Exposure to mercury in the womb can cause brain damage and hearing and vision problems.[37] |
| Radiation | Exposure to radiation during pregnancy (especially between 2 and 18 weeks of pregnancy) can slow growth, cause birth defects, affect brain development, cause cancer, and cause miscarriage.[38] |
| Solvents | These chemicals include degreasers, paint thinners, stain and varnish removers, paints, and more Maternal inhalation of solvents can cause fetal exposure than may cause miscarriage, slow fetal growth, premature birth, and birth defects.[39] |
Maternal Infections as Teratogens
Teratogens from Pets and Other Animals
Toxoplasmosis: The tiny parasite, toxoplasma gondii, causes an infection called toxoplasmosis. According to the March of Dimes (2012d), toxoplasma gondii infects more than 60 million people in the United States. A healthy immune system can keep the parasite at bay producing no symptoms, so most people do not know they are infected. As a routine prenatal screening frequently does not test for the presence of this parasite, pregnant women may want to talk to their health-care provider about being tested. Toxoplasmosis can cause premature birth, stillbirth, and can result in birth defects to the eyes and brain. While most babies born with this infection show no symptoms, ten percent may experience eye infections, enlarged liver and spleen, jaundice, and pneumonia. To avoid being infected, women should avoid eating undercooked or raw meat and unwashed fruits and vegetables, touching cooking utensils that touched raw meat or unwashed fruits and vegetables, and touching cat feces, soil or sand. If women think they may have been infected during pregnancy, they should have their baby tested.
Teratogens from Pets/Animals
| Teratogen | Potential Effects |
| Toxoplamosis | This parasite can be passed through cat feces and undercooked meat (especially pork, lamb, or deer meet). If the fetus is infected it can cause miscarriage, stillbirth, hydrocephalus, macro or microcephalus, vision issues, and damage to the nervous system.[40] |
| Lymphocytic choriomeningitis | This virus carried by rodents including mice, hamsters, and guinea pigs. If an infected mother passes it to her fetus it can cause issues with brain development, long-term neurological and/or visual impairment, and higher mortality rates after birth.[41] |
Sexually Transmitted Diseases
Gonorrhea, syphilis, and chlamydia are sexually transmitted infections that can be passed to the fetus by an infected mother. Mothers should be tested as early as possible to minimize the risk of spreading these infections to their unborn child. Additionally, the earlier the treatment begins, the better the health outcomes for mother and baby (CDC, 2016d). Sexually transmitted diseases (STDs) can cause premature birth, premature rupture of the amniotic sac, an ectopic pregnancy, birth defects, miscarriage, and still births (March of Dimes, 2013). Most babies become infected with STDS while passing through the birth canal during delivery, but some STDs can cross the placenta and infect the developing fetus.
Human Immunodeficiency Virus (HIV)
One of the most potentially devastating teratogens is HIV. HIV and Acquired Immune Deficiency Syndrome (AIDS) are leading causes of illness and death in the United States (Health Resources and Services Administration, 2015). One of the main ways children under age 13 become infected with HIV is via mother-to-child transmission of the virus prenatally, during labor, or by breastfeeding (CDC, 2016c). There are some measures that can be taken to lower the chance the child will contract the disease. HIV positive mothers who take antiviral medications during their pregnancy greatly reduce the chance of passing the virus to the fetus. The risk of transmission is less than 2 percent; in contrast, it is 25 percent if the mother does not take antiretroviral drugs (CDC, 2016b). However, the long-term risks of prenatal exposure to the medication are not known. It is recommended that women with HIV deliver the child by c-section, and that after birth they avoid breast feeding.
German measles (or rubella)
Rubella, also called German measles, is an infection that causes mild flu-like symptoms and a rash on the skin. However, only about half of children infected have these symptoms, while others have no symptoms (March of Dimes, 2012a). Rubella has been associated with a number of birth defects. If the mother contracts the disease during the first three months of pregnancy, damage can occur in the eyes, ears, heart or brain of the unborn child. Deafness is almost certain if the mother has German measles before the 11th week of prenatal development and can also cause brain damage. Women in the United States are much less likely to be afflicted with rubella, because most women received childhood vaccinations that protect her from the disease.[42]
Maternal Infections as Teratogens
| Teratogen | Potential Effects |
| Rubella | Congenital infection (becoming infected while in the womb) can damage the development of the eyes, ears, heart, and brain and result in deafness.[43] |
| Zika | Congenital infection can cause microcephaly and other severe brain abnormalities.[44] |
| Varicella (chicken pox) | Congenital infection can cause a severe form of the infection affecting the eyes, limbs, skin, and central nervous system.[45] |
| Sexually transmitted infections | Infections such as HIV, gonorrhea, syphilis, and chlamydia can be passed from the mother during pregnancy and/or delivery.[46] |
| Listeria | Pregnant women are more susceptible to this food-borne illness. Congenital infection can cause miscarriage, stillbirth, premature labor, and neonatal sepsis.[47] |
Other Maternal Factors
There are additional factors that affect the outcome of pregnancy for both mother and child. Let’s look at these next.
Mothers over 35
Most women over 35 who become pregnant are in good health and have healthy pregnancies. However, according to the March of Dimes (2016d), women over age 35 are more likely to have an increased risk of:
- Fertility problems
- High blood pressure
- Diabetes
- Miscarriages
- Placenta Previa
- Cesarean section
- Premature birth
- Stillbirth
- A baby with a genetic disorder or other birth defects
Because a woman is born with all her eggs, environmental teratogens can affect the quality of her eggs as a woman gets older. Also, a woman’s reproductive system ages which can adversely affect the pregnancy. Some women over 35 choose special prenatal screening tests, such as a maternal blood screening, to determine if there are any health risks for the baby.
Although there are medical concerns associated with having a child later in life, there are also many positive consequences to being a more mature parent. Older parents are more confident, less stressed, and typically married, providing family stability. Their children perform better on math and reading tests, and they are less prone to injuries or emotional troubles (Albert, 2013). Women who choose to wait are often well educated and lead healthy lives. According to Gregory (2007), older women are more stable, demonstrate a stronger family focus, possess greater self-confidence, and have more money. Having a child later in one’s career equals overall higher wages. In fact, for every year a woman delays motherhood, she makes 9% more in lifetime earnings. Lastly, women who delay having children live longer.[48]
Teenage Pregnancy
A teenage mother is at a greater risk for having pregnancy complications including anemia, and high blood pressure. These risks are even greater for those under age 15. Infants born to teenage mothers have a higher risk for being premature and having low birthweight or other serious health problems. Premature and low birthweight babies may have organs that are not fully developed which can result in breathing problems, bleeding in the brain, vision loss, and serious intestinal problems. Very low birthweight babies (less than 3 1/3 pounds) are more than 100 times as likely to die, and moderately low birthweight babies (between 3 1/3 and 5 ½ pounds) are more than 5 times as likely to die in their first year, than normal weight babies (March of Dimes, 2012c). Again, the risk is highest for babies of mothers under age 15. Reasons for these health issues include that teenagers are the least likely of all age groups to get early and regular prenatal care. Additionally, they may engage in negative behaviors including eating unhealthy food, smoking, drinking alcohol, and taking drugs. Additional concerns for teenagers are repeat births. About 25% of teen mothers under age 18 have a second baby within 2 years after the first baby’s birth.
Gestational Diabetes
Seven percent of pregnant women develop gestational diabetes (March of Dimes, 2015b). Diabetes is a condition where the body has too much glucose in the bloodstream. Most pregnant women have their glucose level tested at 24 to 28 weeks of pregnancy. Gestational diabetes usually goes away after the mother gives birth, but it might indicate a risk for developing diabetes later in life. If untreated, gestational diabetes can cause premature birth, stillbirth, the baby having breathing problems at birth, jaundice, or low blood sugar. Babies born to mothers with gestational diabetes can also be considerably heavier (more than 9 pounds) making the labor and birth process more difficult. For expectant mothers, untreated gestational diabetes can cause preeclampsia, a complication that results in high blood pressure and signs of damage to other organs, most commonly the liver and kidneys. Risk factors for gestational diabetes include age (being over age 25), being overweight or gaining too much weight during pregnancy, family history of diabetes, having had gestational diabetes with a prior pregnancy, and race and ethnicity (African-American, Native American, Hispanic, Asian, or Pacific Islander have a higher risk). Eating healthy and maintaining a healthy weight during pregnancy can reduce the chance of gestational diabetes. Women who already have diabetes and become pregnant need to make sure to attend all their prenatal care visits, and follow the same advice as those for women with gestational diabetes as the risk of preeclampsia, premature birth, birth defects, and stillbirth are the same.
High Blood Pressure (Hypertension)
Hypertension is a condition in which the pressure against the wall of the arteries becomes too high. There are two types of high blood pressure that can result during pregnancy, gestational and chronic. Gestational hypertension only occurs during pregnancy and goes away after birth. Chronic high blood pressure refers to women who already had hypertension before the pregnancy or to those who developed it during pregnancy, and it continued after birth. According to the March of Dimes (2015c) about 8 in every 100 pregnant women have high blood pressure. High blood pressure during pregnancy can cause premature birth and low birth weight (under five and a half pounds), placental abruption, and preeclampsia.
Rh Disease
Rh is a protein found in the blood. Most people are Rh positive, meaning they have this protein. Some people are Rh negative, meaning this protein is absent. Mothers who are Rh negative are at risk of having a baby with a form of anemia called Rh disease (March of Dimes, 2009). A father who is Rh-positive and mother who is Rh-negative can conceive a baby who is Rh-positive. In this case, some of the fetus’s blood cells may get into the mother’s bloodstream and her immune system is unable to recognize the Rh factor. The immune system starts to produce antibodies to fight off what it thinks is a foreign invader. Once her body produces immunity, the antibodies can cross the placenta and start to destroy the red blood cells of the developing fetus. As this process takes time, often the first Rh positive baby is not harmed, but as the mother’s body will continue to produce antibodies to the Rh factor across her lifetime, subsequent pregnancies can pose greater risk for an Rh positive baby. In the newborn, Rh disease can lead to jaundice, anemia, heart failure, brain damage and death.
Weight Gain during Pregnancy
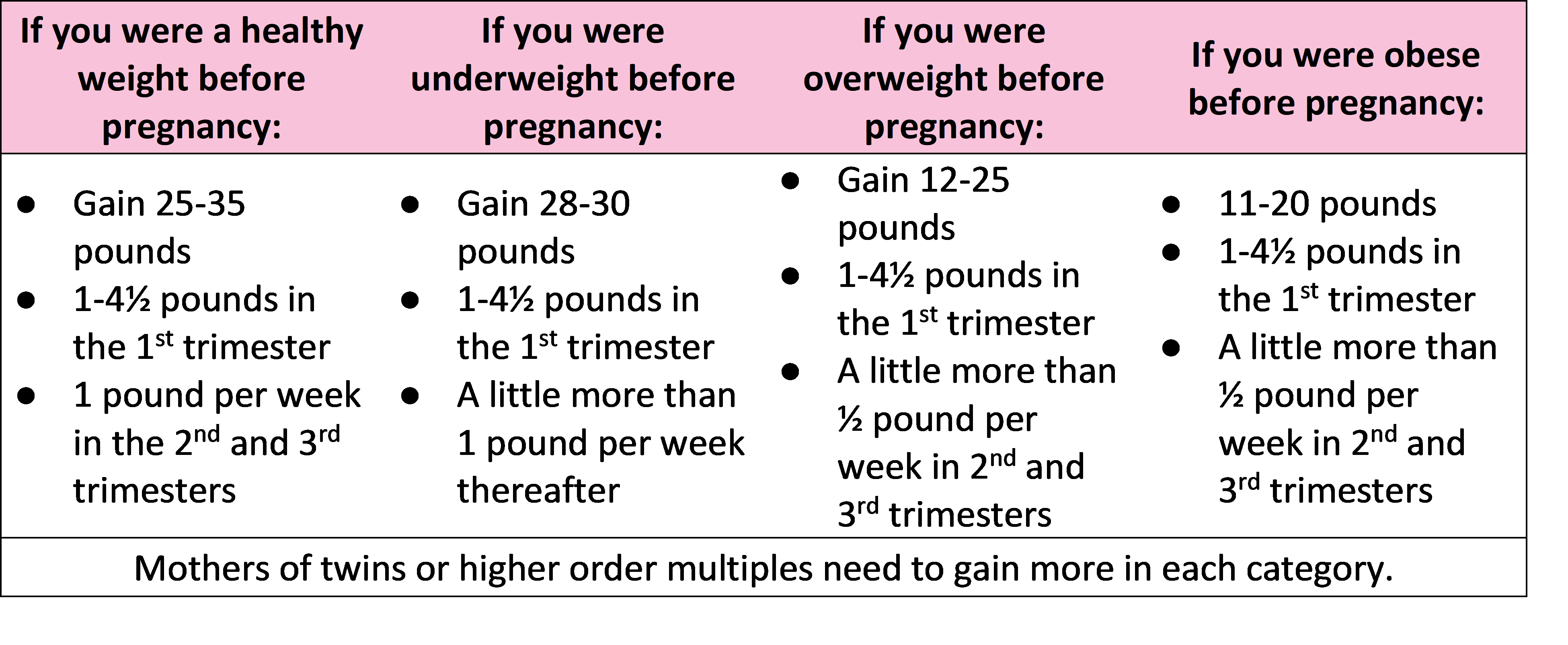
According to March of Dimes (2016f) during pregnancy most women need only an additional 300 calories per day to aid in the growth of the fetus. Gaining too little or too much weight during pregnancy can be harmful. Women who gain too little weight may have a baby who is low-birth weight, while those who gain too much are likely to have a premature or large baby. There is also a greater risk for the mother developing preeclampsia and diabetes, which can cause further problems during the pregnancy, so putting on the weight slowly is best. Mothers who are concerned about their weight gain should talk to their health care provider.[49] The table below shows healthy weight gain during pregnancy.
Weight Gain During Pregnancy[50]
 Stress
Stress
Feeling stressed is common during pregnancy, but high levels of stress can cause complications including having a premature baby or a low-birthweight baby. Babies born early or too small are at an increased risk for health problems. Stress-related hormones may cause these complications by affecting a woman’s immune systems resulting in an infection and premature birth. Additionally, some women deal with stress by smoking, drinking alcohol, or taking drugs, which can lead to problems in the pregnancy. High levels of stress in pregnancy have also been correlated with problems in the baby’s brain development and immune system functioning, as well as childhood problems such as trouble paying attention and being afraid (March of Dimes, 2012b).
Depression: Depression is a significant medical condition in which feelings of sadness, worthlessness, guilt, and fatigue interfere with one’s daily functioning. Depression can occur before, during, or after pregnancy, and 1 in 7 women is treated for depression sometime between the year before pregnancy and year after pregnancy (March of Dimes, 2015a). Women who have experienced depression previously are more likely to have depression during pregnancy. Consequences of depression include the baby being born premature, being low birthweight, being more irritable, less active, less attentive, and having fewer facial expressions. About 13% of pregnant women take an antidepressant during pregnancy. It is important that women taking antidepressants during pregnancy discuss the medication with a health care provider as some medications can cause harm to the developing organism. In fact, birth defects happen about 2 to 3 times more often in women who are prescribed certain Selective Serotonin Reuptake Inhibitors (SSRIs) for their depression.
Paternal Impact
The age of fathers at the time of conception is also an important factor in health risks for children. According to Nippoldt (2015) offspring of men over 40 face an increased risk of miscarriages, autism, birth defects, achondroplasia (bone growth disorder) and schizophrenia. These increased health risks are thought to be due to accumulated chromosomal aberrations and mutations during the maturation of sperm cells in older men (Bray, Gunnell, & Smith, 2006). However, like older women, the overall risks are small.
In addition, men are more likely than women to work in occupations where hazardous chemicals, many of which have teratogenic effects or may cause genetic mutations, are used (Cordier, 2008). These may include petrochemicals, lead, and pesticides that can cause abnormal sperm and lead to miscarriages or diseases. Men are also more likely to be a source of secondhand smoke for their developing offspring. As noted earlier, smoking by either the mother or around the mother can hinder prenatal development.[51]
Test Yourself
Prenatal Assessment
A number of assessments are suggested to women as part of their routine prenatal care to find conditions that may increase the risk of complications for the mother and fetus (Eisenberg, Murkoff, & Hathaway, 1996). These can include blood and urine analyses and screening and diagnostic tests for birth defects.
Ultrasound is one of the main screening tests done in combination with blood tests. The ultrasound is a test in which sound waves are used to examine the fetus. There are two general types. Transvaginal ultrasounds are used in early pregnancy, while transabdominal ultrasounds are more common and used after 10 weeks of pregnancy (typically, 16 to 20 weeks). [52]
Transvaginal Ultrasound
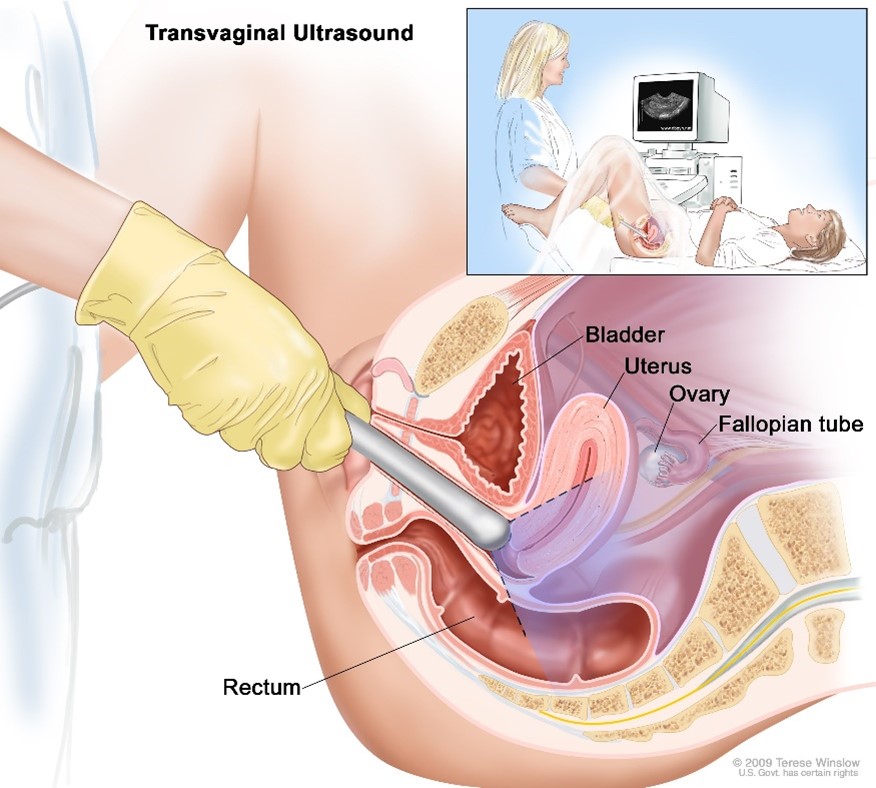
Transvaginal ultrasound. An ultrasound probe connected to a computer is inserted into the vagina and is gently moved to show different organs. The probe bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture).[53]
Transabdominal Ultrasound[54]

Ultrasounds are used to check the fetus for defects or problems. It can also find out the age of the fetus, location of the placenta, fetal position, movement, breathing and heart rate, amount of amniotic fluid in the uterus, and number of fetuses. Most women have at least one ultrasound during pregnancy, but if problems are noted, additional ultrasounds may be recommended.[55]
4-D Ultrasound of a Fetus Yawning[56]

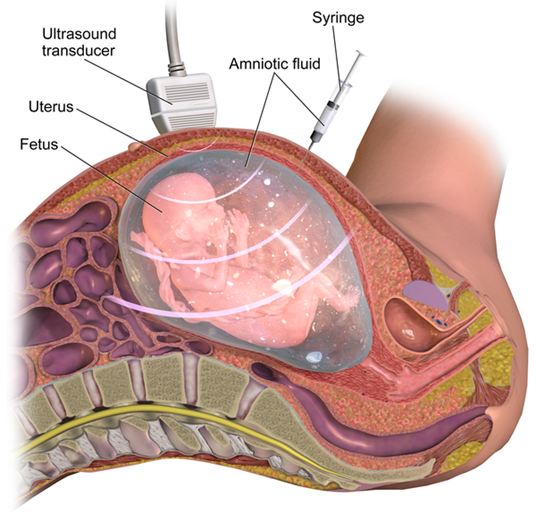
When diagnosis of a birth defect is necessary, ultrasounds help guide the more invasive diagnostic tests of amniocentesis and chorionic villus sampling. Amniocentesis is a procedure in which a needle is used to withdraw a small amount of amniotic fluid and cells from the sac surrounding the fetus and later tested.[57]
Amniocentesis[58]
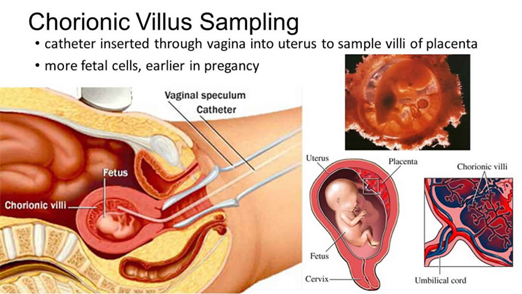
Chorionic Villus Sampling
The chorion is the portion of fetal membrane that eventually forms the fetal side of the placenta. The chorion contains chorionic villi, which are small finger-like projections. These villi are snipped or suctioned off for study in the procedure. Since the chorionic villi are of fetal origin, examining samples of them can provide the genetic makeup of the fetus. This test is performed to identify congenital defects. Experts use the sample to study the DNA, chromosomes, and enzymes of the fetus. The test can be done before amniocentesis, about 10 to 12 weeks after a missed period.[59]
CVS can be done through the cervix (transcervical) or through the belly (transabdominal). Miscarriage rates are slightly higher when the test is done through the cervix.
The transcervical procedure is performed by inserting a thin plastic tube through the vagina and cervix to reach the placenta. Your health care provider uses ultrasound images to help guide the tube into the best area for sampling. A small sample of chorionic villus (placental) tissue is then removed.
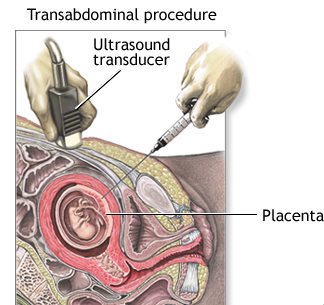
The transabdominal procedure is performed by inserting a needle through the abdomen and uterus and into the placenta. Ultrasound is used to help guide the needle, and a small amount of tissue is drawn into the syringe.[60]
Transcervical Chorionic Villus Sampling[61]
Transabdominal Chorionic Villus Sampling[62]
First-Trimester Screening
A first-trimester screening combines the use of transabdominal ultrasound and a blood test during the first trimester of pregnancy (week 1 through 13), and is usually done between week’s 11 and 13. Using ultrasound a Nuchal Translucency Test is performed to measure the amount of fluid and thickness around the area of the back of the baby’s neck (this area is called the nuchal fold). This test can determine if there is a chance of certain birth defects like Down’s Syndrome, Patau’s Synderome (trisomy 13), and Edward’s Syndrome (trisomy 18) being present. However, the nuchal translucency screening on its own is not good enough to make a diagnosis. The Nuchal translucency test correctly identifies Down Syndrome in approximately 64 to 70 percent of the time but fails to identify Down’s Syndrome approximately 30 to 36 percent of the time. To improve the accuracy of the nuchal translucency screening, two blood tests will also be taken.
Ultrasound of 13-Week Old Fetus

Ultrasound image of measurements of fetal nuchal translucency at 13 weeks. The area marked NT on the ultrasound image shows the Nuchal fold area which is measured for fluid and thickness. Babies with increased fluid in this area are at a higher risk for having Down’s Syndrome, Patau’s Syndrome (trisomy 13), and Edward’s Syndrome (trisomy 18). A normal measurement of the nuchal fold at 13 weeks is approximately 3mm.[63]
The blood tests measure two different substances that are found in the blood of all pregnant women, the pregnancy-associated plasma protein or (PAPP-A) and human-chorionic gonadotropin (Beta-hCG). PAPP-A is a protein produced by the placenta early in the pregnancy and can be found in the protein of the mom’s blood. Low levels of PAPP-A may be associated with birth defects. Beta-gCG is a hormone produced by the placenta also in early pregnancy. High or low levels of Beta-gCG may be related to certain birth defects. When the PAPP-A and Beta-gCG blood tests are combined with the results of the Nuchal translucency test the combined results correctly identifies Down’s syndrome approximately 82 to 87 percent of the time. A quad screening (another type of blood test) performed during the second trimester increases the ability to detect Down’s Syndrome to approximately 96%.
Test Yourself
Complications of Pregnancy
Minor Complications
There are a number of common side effects of pregnancy. Not everyone experiences all of these, nor to the same degree. And although they are considered “minor” this is not to say that these problems are not potentially very uncomfortable. These side effects include nausea (particularly during the first 3-4 months of pregnancy as a result of higher levels of estrogen in the system), heartburn, gas, hemorrhoids, backache, leg cramps, insomnia, constipation, shortness of breath or varicose veins (as a result of carrying a heavy load on the abdomen).
Major Complications
The following are some serious complications of pregnancy which can pose health risks to mother and child and that often require hospitalization.
Spontaneous abortion is experienced in an estimated 20-40 percent of undiagnosed pregnancies and in another 10 percent of diagnosed pregnancies. Usually, the brts due to chromosomal abnormalities, and this typically happens before the 12th week of pregnancy. Cramping and bleeding result and normal periods return after several months. Some women are more likely to have repeated miscarriages due to chromosomal, amniotic, or hormonal problems, but miscarriage can also be a result of defective sperm (Carrell et. al., 2003).[64]
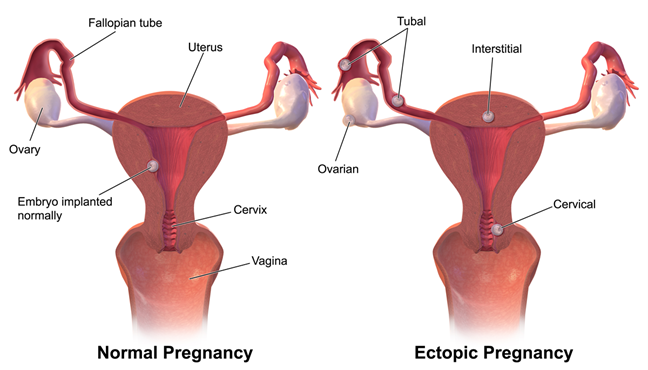
An Ectopic Pregnancy occurs when an embryo grows outside the womb. In most ectopic pregnancies (approximately 90%), the embryo attaches to a fallopian tube before it reaches the uterus. Less often, it attaches to an ovary, the cervix or to the myometrium, all of which are areas that do not have enough space or the right tissue for the embryo to grow. Without treatment, an ectopic pregnancy can cause serious bleeding and even maternal death, and all ectopic pregnancies end in pregnancy loss.[65]
According to the March of Dimes about 1 in 50 pregnancies (2 percent) in the United States is ectopic, however the estimated rate of ectopic pregnancy in the general population is 1 to 2% and 2 to 5% among patients who utilized assisted reproductive technology. However about 1 in 3 women (33 percent) who have had one ectopic pregnancy go on to have a healthy pregnancy later.
Illustration of Normal Implantation of the Zygote and Four Possible Ectopic Pregnancy Areas[66]
Hyperemesis gravidarum is characterized by severe nausea, vomiting, weight loss, and possibly dehydration. Signs and symptoms may also include vomiting many times a day and feeling faint. The exact causes of hyperemesis gravidarum are unknown. Risk factors include the first pregnancy, multiple pregnancy, obesity, prior or family history of HG, trophoblastic disorder, and a history of eating disorders. Treatment includes drinking fluids and a bland diet. Medication, intravenous fluids, and hospitalization may be required. Hyperemesis gravidarum is estimated to affect 0.3–2.0% of pregnant women. Those affected have a low risk of miscarriage but a higher risk of premature birth.
Preeclampsia (briefly discussed earlier in the chapter) , also known as Toxemia, is characterized by a sharp rise in blood pressure, a leakage of protein into the urine as a result of kidney problems, and swelling of the hands, feet, and face during the third trimester of pregnancy. Preeclampsia is the most common complication of pregnancy. It is estimated to affect 5% to 10% of all pregnancies globally and accounts for 40% to 60% of maternal deaths in developing countries (National Institute of Child Health and Human Development, 2013). Rates are lower in the United States and preeclampsia affects about 3% to 5% of pregnant women.
Preeclampsia occurs most frequently in first pregnancies, and it is more common in women who are obese, have diabetes, or are carrying twins. When preeclampsia causes seizures, the condition is known as eclampsia, which is the second leading cause of maternal death in the United States. Preeclampsia is also a leading cause of fetal complications, which include low birth weight, premature birth, and stillbirth. Treatment is typically bed rest and sometimes medication. If this treatment is ineffective, labor may be induced.
Maternal Mortality: According to the CDC (2019), about 700 American women die from complications related to pregnancy each year, and this number is rising. Further, 60% of those deaths could have been prevented. Bleeding, infections, and heart-related problems are the main causes. Possible contributing factors include the high caesarean section rate and obesity. Compared to other developed nations, this number is considered high. Approximately 1000 women die in childbirth around the world each day (World Health Organization, 2010). Rates are highest in Sub-Saharan Africa and South Asia, although there has been a substantial decrease in these rates. The campaign to make childbirth safe for everyone has led to the development of clinics accessible to those living in more isolated areas and training more midwives to assist in childbirth.
Test Yourself
Infertility and Building Families
Infertility
Healthcare providers consider a couple infertile if they try but fail to get pregnant within one year. When the woman is older than 35, the amount of time trying to conceive drops to six months for an infertility diagnosis. In women over 40, immediate evaluation is warranted. Infertility does not include miscarrying or being unable to carry a baby to childbirth. There are two types of infertility. Primary infertility defines a woman who was never pregnant and who can’t conceive after on year of not using birth control, whereas secondary infertility occurs when a woman can’t get pregnant again after having at least one successful pregnancy. Women who lose the baby before the 20th week of pregnancy experience what is called a miscarriage or spontaneous abortion, while a woman who loses the baby after 20 weeks of pregnancy experience what is called a stillbirth.[67]
Infertility affects about 6.7 million women or 11 percent of the reproductive age population (American Society of Reproductive Medicine [ASRM], 2006-2010. Male factors create infertility in about a third of the cases. For men, the most common cause is a lack of sperm production or low sperm production. Female factors cause infertility in another third of cases. For women, one of the most common causes of infertility is ovulation disorder. Other causes of female infertility include blocked fallopian tubes, which can occur when a woman experiences abnormal uterine tissue growth as in endometriosisor resulting from an infection such as pelvic inflammatory disease (PID). PID is experienced by 1 out of 7 women in the United States and leads to infertility about 20 percent of the time. One of the major causes of PID is chlamydia, the most commonly diagnosed sexually transmitted infection in young women. Another cause of pelvic inflammatory disease is gonorrhea. Both male and female factors contribute to the remainder of cases of infertility and approximately 20 percent are unexplained.[68]
Options for Building Families
Assisted Reproductive Technology
Assisted Reproductive Technology (ART) is the technology used to achieve pregnancy in procedures such as fertility medication (to stimulate ovulation), surgical procedures, artificial insemination IUI), in vitro fertilization (IVF) and surrogacy. These options are available for people who are experiencing infertility or cannot conceive children naturally (which also includes single parents, and gay/lesbian couples).[69]
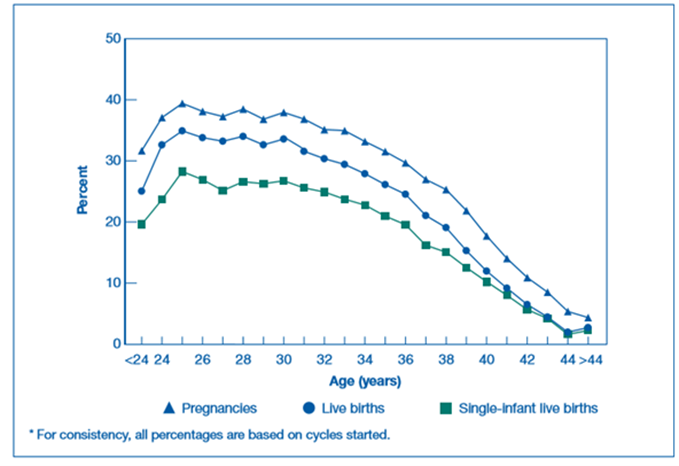
Percentages of ART Cycles Using Fresh Embryos from Fresh Nondonor Eggs That Resulted in Pregnancies, Live Births, and Single-Infant Live Births, by Age of Woman (2016) [70]
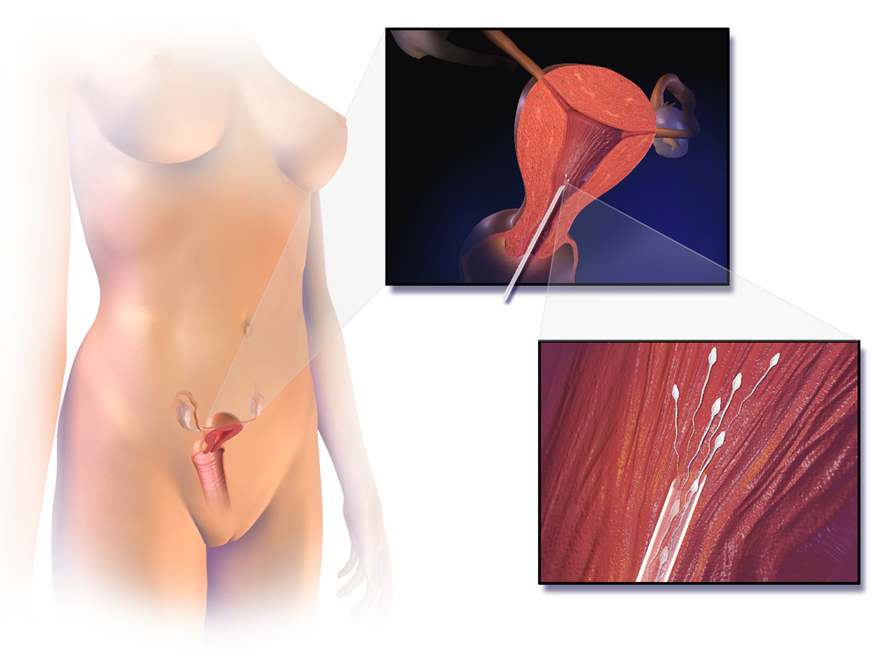
Artificial Insemination (AI)/Intrauterine Insemination (IUI)
Artificial insemination (AI) or intrauterine insemination (IUI) is the deliberate introduction of sperm into a female’s cervix or uterine cavity for the purpose of achieving a pregnancy through in vivo fertilization by means other than sexual intercourse. AI is most often used by single women who desire to give birth to their own child, women who are in a lesbian relationship, or women who are in a heterosexual relationship but with a male partner who is infertile or who has a physical impairment which prevents intercourse. The sperm used could be anonymous or from a known donor.[71]
Artificial Insemination/Intrauterine Insemination (IUI) Procedure[72]
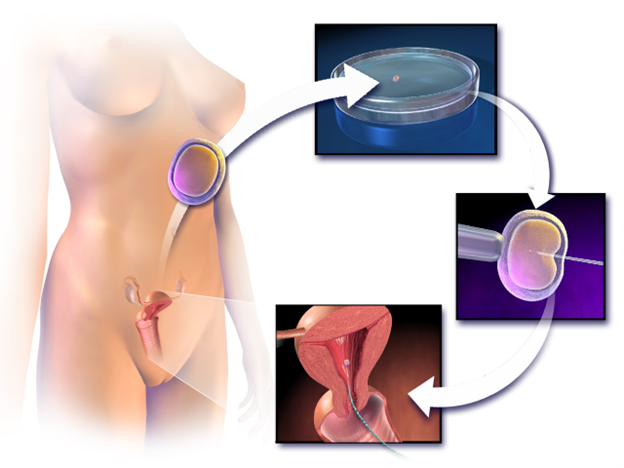
In vitro fertilization (IVF)
A common type of assisted reproductive technology is in vitro fertilization (IVF) where an egg and sperm are combined outside the body and then placed in the uterus. Eggs are obtained from the woman after extensive hormonal treatments that prepare mature eggs for fertilization and prepare the uterus for implantation of the fertilized egg. Sperm are obtained from the male and combined with the eggs, which are then supported through several cell divisions to ensure viability of the zygotes. When the embryos have reached the eight-cell stage, one or more is implanted into the woman’s uterus. If fertilization is not accomplished by simple IVF, a procedure known as intracytoplasmic sperm injection (ICSI) can be used to inject the sperm into an egg. IVF procedures produce a surplus of fertilized eggs and embryos that can be frozen and stored for future use; the procedures can also result in multiple births[73]
The IVF Process[74]
Donor Gametes & Embryos
People can also use sperm, ova (eggs), and embryos from donors in conjunction with ART. These donations take place through agencies and donor banks or between private individuals. In the U.S., donors can be compensated for their donations.
Surrogacy
In surrogacy, one woman (surrogate mother) carries a child for another person/s (commissioning person/couple), based on a legal agreement before conception requiring the child to be relinquished to the commissioning person/couple following birth. There are different types of surrogacies which relate to whether or not the ova used to conceive the child are her own (traditional surrogacy) or not (gestational surrogacy).[75]
Adoption
People can also choose to pursue adoption to build their families (with or without experiencing infertility). Adoption can take place through the foster care system, privately, or through agencies. Adoptions can be domestic (within the U.S.) or international. And they can be open (with differing amounts of contact between biological/birth families and adoptive families) or closed.
Test Yourself
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image and above text from "Concepts of Biology- 1st Canadian Edition" by Charles Molnar and Jane Gair is licensed under CC BY 4.0 Edits by Maria Pagano ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0. Modified by Maria Pagano ↵
- Image from Wikimedia Commons. Human Fertilization, by Ttrue12. Licensed under CC BY SA 3.0. ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image from Wikipedia and is licensed under CC BY-NC-SA 3.0 ↵
- "Concepts of Biology- 1st Canadian Edition" by Charles Molnar and Jane Gair is licensed under CC BY 4.0 ↵
- "Concepts of Biology- 1st Canadian Edition" by Charles Molnar and Jane Gair is licensed under CC BY 4.0 ↵
- "Concepts of Biology- 1st Canadian Edition" by Charles Molnar and Jane Gair is licensed under CC BY 4.0 ↵
- Image by lunar caustic is licensed under CC BY 2.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective (pages 44-45) by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by CNX Psychology is licensed under CC BY 4.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image is in the public domain ↵
- Image by Jennifer Paris used with permission ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Text and image from Wikipedia and is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by Laura Overstreet is licensed under CC BY-NC-SA 3.0 ↵
- The Embryo Project Encyclopedia by Chanapa Tantibanchachai is licensed under CC BY-NC-SA 3.0; modified by Maria Pagano ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- What Are Fetal Alcohol Spectrum Disorders? Published by The Duke University Pharmacology Education Partnership. Public Domain ↵
- Staying healthy and safe by OWH is in the public domain ↵
- Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0; Staying healthy and safe by OWH is in the public domain ↵
- Staying healthy and safe by OWH is in the public domain ↵
- Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0; Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0; Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0 ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal-products.aspx ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0 ↵
- Protocols on prenatal care for pregnant women with Zika infection and children with microcephaly: nutritional approach by Rachel de Sá Barreto Luna Callou Cruz, Malaquias Batista Filho, Maria de Fátima Costa Caminha, and Edvaldo da Silva Souza is licensed under CC BY 4.0 ↵
- Congenital Varicella syndrome by WikiDoc is licensed under CC BY-SA 3.0 ↵
- Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0 ↵
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2860824/ ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Children’s Development by Ana R. Leon is licensed under ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image and text from National Institute of Health, National Cancer Institute Dictionary of Cancer Terms. Public Domain. ↵
- Image by MedicalPrudens is licensed under CC0 1.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by Wolfgand Moroder.theora.ogv and is licensed under CC BY SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Image by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Courtesy of MedlinePlus from the National Library of Medicine ↵
- Courtesy of MedlinePlus from the National Library of Medicine ↵
- Image courtesy of Health JADE as fair use ↵
- Courtesy of MedlinePlus from the National Library of Medicine ↵
- Image and text (modified by Maria Pagano) from Wikimedia Commons: File: Nuchal translucency Dr. Wolfgang Moroder. Licensed under CC-BY-SA 3.0 ↵
- Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 ↵
- Mummert T, Gnugnoli DM. Ectopic Pregnancy. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Licensed under CC BY 4.0 Edited by Maria Pagano ↵
- Image from Wikipedia: Ectopic Pregnancy is licensed under CC BY SA ↵
- Lifespan Development: A Psychological Perspective (page 57) by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0 Modified by Maria Pagano ↵
- From Lumen Learning Lifespan Development. Authored by: Margaret Clark-Plaskie for Lumen Learning. Licensed under CC BY 4.0 ↵
- Assisted Reproductive Technology by Fertilitypedia is licensed under CC BY-SA 4.0 ↵
- Centers for Disease Control and Prevention, American Society for Reproductive Medicine, society for Assisted Reproductive Technology. 2016 Assisted Reproductive Technology National Summary Report. Atlanta (GA): US Dept. of Health and Human Services;2018 ↵
- From Lumen Learning Lifespan Development. Authored by: Margaret Clark-Plaskie for Lumen Learning. Licensed under CC BY SA 4.0 ↵
- Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. ↵
- Assisted Reproductive Technology by Fertilitypedia is licensed under CC BY-SA 4.0 ↵
- Image by Manu5 is licensed under CC BY-SA 4.0 ↵
- Surrogacy by Fertilitypedia is licensed under CC BY-SA 4.0 ↵
begins at conception when the sperm and egg cell unite in one of the two fallopian tubes and ends when the zygote implants into the uterine wall approximately 2 weeks after conception.
begins with implantation of the zygote into the uterine wall and lasts through the eighth week following fertilization, after which the embryo is called a fetus.
begins at approximately week nine and lasts approximately 30 weeks.
containing two complete sets of chromosomes, one from each parent.
the thick transparent membrane surrounding a mammalian ovum (egg) before implantation.
a membrane-bound cell organelle that contains digestive enzymes
a unique membranous organelle located over the anterior part of the sperm nucleus that contains a number of hydrolytic enzymes that, when secreted, help the sperm penetrate the egg's coats.
the fusion of the acrosomal membrane with the sperm's plasma membrane
having a single set of unpaired chromosomes.
a type of cell division that results in two daughter cells each having the same number and kind of chromosomes as the parent nucleus, typical of ordinary tissue growth.
treatment in which a female patient's eggs are surgically removed from the ovaries fertilized in a laboratory, with sperm from a male partner or sperm donor, to create embryos.
the fertilized egg at the 5th or 6th day after conception is known as a blastocyst — a rapidly dividing ball of cells.
the portion of the blastocyst that will become the embryo.
A thin layer of cells that helps a developing embryo attach to the wall of the uterus, protects the embryo, and forms a part of the placenta.
human offspring during the period from approximately the second to the eighth week after fertilization.
an early developmental process in which an embryo transforms from a one-dimensional layer of cells (blastula) and reorganizes into a multilayered and multidimensional structure.
each of the three layers of cells (ectoderm, mesoderm, and endoderm) that are formed in the early embryo.
The process during which young, immature (unspecialized) cells take on individual characteristics and reach their mature (specialized) form and function.
cells derived from the inner cell mass of the blastocyst prior to implantation. They are pluripotent (capable of giving rise to several different cell types and have an unlimited capacity for self-renewal and the ability to differentiate into any somatic cell type
the general pattern of physical and motoric development followed from infancy into toddlerhood and even early childhood whereby development follows a head-to-toe progression.
the general tendency for the development of motor skills to start at the center of an organism and radiate outwards from there.
unborn baby more than eight weeks after conception.
Any of the cells that hold nerve cells in place and help them work the way they should. Smaller than neurons and typically do not have an axon or dendrite.
provide nourishment for the oocytes during the early stages of their growth
cells from which all other cells with specialized functions are generated.
a thickened portion of ectoderm along the midline of the embryo that forms the foundation of the central nervous system (the brain and the spinal cord)
the neural plate creases inward until the edges come in contact and fuse thus forming the brain and spinal cord.
a hollow structure from which the brain and spinal cord form.
a specialized cell transmitting nerve impulses.
the process by which new neurons are formed in the brain.
brain structure located deep in the temporal lobe which plays a major role in learning and memory.
a short branched extension of a nerve cell, along which impulses received from other cells at synapses are transmitted to the cell body.
the long threadlike part of a nerve cell along which impulses are conducted from the cell body to other cells.
a network or circuit of biological neurons
the darker tissue of the brain and spinal cord, consisting mainly of nerve cell bodies and branching dendrites.
the paler tissue of the brain and spinal cord, consisting mainly of nerve fibers with their myelin sheaths.
the insulating layer around many axons that increases the speed of conduction of nerve impulses.
Anything that can lead to developmental abnormalities in the developing fetus or embryo.
relating to the metabolism of a living organism.
a pregnancy in which the fetus develops outside the uterus, typically in a fallopian tube.
a condition where the placenta partially or wholly blocks the uterus and interferes with the delivery of the baby.
A substance use to destroy insects.
a chemical compound used in manufacturing plastics such as water bottles.
a form of high blood pressure that occurs during pregnancy.
the term for having high blood pressure.
condition where antibodies in a pregnant woman's blood may detstroy her baby's blood cells.
a hereditary condition that results in very short limbs and sometimes a face that is small in relation to the skull.
a procedure that uses high-energy sound waves to look at tissues and organs inside the body. Can also be used to examine the embryo and fetus.
an examination of the female pelvis, which can determine abnormalities in the uterus, cervix, endometrium (lining of the womb), fallopian tubes, and ovaries.
transmission and reflection of ultrasound waves to visualize internal organs through the abdominal wall.
sampling of amniotic fluid using a needle inserted into the uterus, to screen for developmental abnormalities in a fetus.
a test during pregnancy to detect congenital abnormalities in the fetus by using a tiny tissue sample taken from the villi of the chorion
the outermost membrane surrounding an embryo, contributes to the formation of the placenta.
combines fetal ultrasound and blood tests for the mother which serves as a prenatal test that offers early information about the risk of conditions like Down's Syndrome (trisomy 21) and Edward's Syndrome (trisomy 18).
an ultrasound scan that measures a baby's nuchal translucency — a fluid-filled space behind the baby's neck.
pregnancy loss at less than 20 weeks' gestation
the smooth muscle tissue of the uterus which is involved in contraction during labor.
persistent severe vomiting leading to weight loss and dehydration, as a condition occurring during pregnancy.
a condition in pregnancy characterized by high blood pressure
when a pregnancy has never been achieved by a person
infertility occurs after one prior pregnancy.
also called spontaneous abortion. The unexpected ending of a pregnancy in the first 20 weeks of gestation.
the death or loss of a baby after 20 weeks gestation. Can occur before or during delivery
a condition in which the layer of tissue that normally covers the inside of the uterus, grows outside of it
an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis
a sexually transmitted infection caused by the bacterium chlamydia trachomatis
a sexually transmitted infection (STI) caused by the bacterium neisseria gonorrhoeae
also called intrauterine insemination (IUI). The deliberate introduction of sperm into a female’s cervix in order to become pregnant by means other than sexual intercourse
also called artificial insemination. A procedure for treating infertility where sperm is placed directly into the uterus using a small catheter.
a form of in vitro fertilization where a single sperm is injected into the center of the egg.

